A novel treatment provides higher survival benefit in hard-to-match kidney transplant patients.

Apart from the scarcity of donor kidneys, the biggest barrier to kidney transplant right now is the percentage (nearly one in three) of patients on the waiting list whose immune systems make them likely to reject most kidneys available to them, says Montgomery.Widespread use of a presurgery protocol developed at Johns Hopkins, which removes problematic antibodies from a patient's blood prior to transplant, could lead to potentially 3,000 more kidney transplants from living donors each year, he says. The presurgery process cannot be used at this point with patients receiving cadaver organs because several days of treatment are needed before surgery can take place.
"We have this presurgery therapy that doubles a person's survival rate," says Montgomery, who is also director of Johns Hopkins' Comprehensive Transplant Center. "If this were a cancer drug that doubled chances of survival, people would be lined up out the door to get it. It's really extraordinary to go from 30 percent survival to 80 percent survival after eight years."
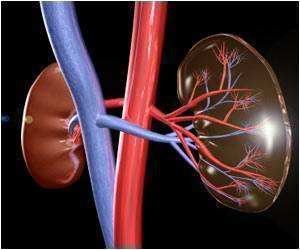
Montgomery estimates that these hard-to-match transplant candidates number more than 20,000 in the United States. Their immune systems will reject most kidneys because of antibodies circulating in their blood that react to proteins known as human leukocyte antigens (HLA). These proteins are found on most cells and are used by the immune system to recognize what is foreign to the body.
In what are known as HLA-sensitized patients, the body has been exposed to foreign HLA in the past, either through pregnancy, blood transfusion or previous kidney transplant, and it immediately recognizes most donor organs as unfamiliar, causing rejection. Women make up a majority of these patients because of sensitization from pregnancy.
Montgomery's new protocol removes the problem antibodies from the blood before the transplant takes place through plasmapheresis, a process that removes, filters and replaces a person's plasma supply. Then, the patient receives low-dose intravenous immune globulin (IVIg), which aims to replace those problematic antibodies and prevent their return. This process, which conditions the body to accept the new organ, is performed every other day for several days before transplant and then for up to 10 days following the surgery. Thereafter, Montgomery says, the patient just needs the same anti-rejection medication as any other transplant patient. In the study, there were very few significant side effects from plasmapheresis.
Historically, highly HLA-sensitized patients have been very difficult to match with fewer than 7 percent receiving transplants each year compared to a dramatic 98 percent transplant rate among patients offered the Johns Hopkins' plasmapheresis protocol.
Montgomery says the protocol, which he and his colleagues at Hopkins pioneered in 1998, essentially allows an incompatible kidney to function long term, and in the majority of patients, the harmful antibodies do not return. Some other hospitals have begun using it, as well, but Montgomery says many others were awaiting data indicating long-term benefit to patients.
"Now we have it, the first study to show long-term survival benefit from desensitization," he says.
In the new research, Montgomery and colleagues transplanted 211 HLA-sensitized patients between February 1998 and December 2009 using plasmapheresis and IVIg before and after surgery. In order to develop a control group, the researchers, on the day each patient received his or her incompatible transplant, identified five patients on the kidney waiting list who most closely matched the characteristics of the person who got the new organ. The researchers then followed the progress of those transplant candidates, as well, whether they remained on dialysis or eventually got a compatible organ.
After the first year, each group of patients had about the same chance for survival (in the low 90 percentile range). After eight years, however, the treatment group had an 80.6 percent survival rate, while the dialysis group had a 30.5 percent chance of survival. The patients who waited on the list with the possibility of receiving a compatible kidney had a 49.1 percent chance of eight-year survival. Montgomery points out that the number of these patients who actually received a compatible transplant was very small because finding compatible organs for HLA-sensitized patients is so challenging.
In 2008, of the 82,000 patients on the waiting list in the United States, 16,520 received kidney transplants whereas 4,800 died waiting for one.
Acknowledging that desensitization makes kidney transplants more expensive, Montgomery says the cost savings when compared to remaining on dialysis are enormous. Meanwhile, the patient no longer has to endure the difficulties of dialysis, a blood-cleansing process that takes about five hours a day, three days a week, and which often makes the tasks of daily life from working to caring for children nearly impossible.
"This treatment increases survival, ensures a better lifestyle and saves the health care system money," he says. "There aren't many things like that."
Montgomery says he expects his findings to significantly ease doubts about the ability of HLA-sensitized candidates to have successful transplants. In many parts of the country, he says, insurers who historically have not covered desensitization should now reconsider.
Source-Eurekalert