Myotonic dystrophy type 1 (DM1) is the most common inherited muscular dystrophy in adults. New research published by Cell Press online on March 31st in the journal Cell Stem

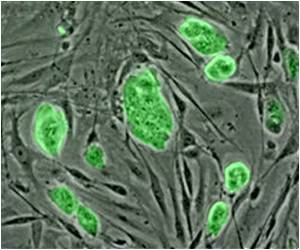
"We used pluripotent stem cell lines derived from human embryos characterized during preimplantation genetic diagnosis as carrying the gene for DM1," explains senior study author, Dr. Martinat. "These cells can self-renew indefinitely, making them available in large numbers, and they possess the ability to differentiate into any type of cell, allowing us to perform key functional studies."
The researchers looked at neural cells made from their embryonic stem cell lines, and found reduced expression of genes in the SLITRK family that was mirrored in brain biopsies from DM1 patients. SLITRK proteins are involved in the outgrowth of neurons and the formation of synapses, which are sites of communication between nerve and muscle cells. Martinat and colleagues looked at DM1 neurons cultured together with muscle cells, and found that the change in SLITRK expression caused defects in the cell-cell connections that formed.
"These neuropathological mechanisms may be clinically significant for the functional changes in neuromuscular connections associated with DM1," says Dr. Martinat. "In addition, our results highlight the tremendous value of human pluripotent stem cells as an appropriate model to decipher events involved in the pathogenesis of a disease state. This is especially relevant now, as the French Parliament voted in favor of a revised bioethics bill last February that will restrict embryo research." says Dr.Marc Peschanski, Head of I-Stem. In support of successful pathological models like the one described here, a broad consensus of researchers and clinicians is now urging the French Senate to overturn the ban in a vote scheduled for April 5th, and to explicitly authorize research on human embryonic stem cells.
Source-Eurekalert