Peripheral arterial disease (PAD) may be a signal of future heart attack and stroke, says study. PAD is a common condition affecting 12-20 percent of Americans age 65 and older.
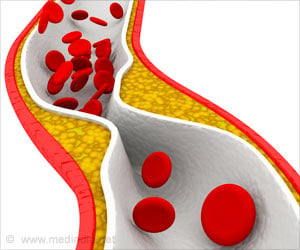
An estimated 10 million people in the United States suffer from peripheral arterial disease. PAD develops mostly as a result of atherosclerosis, a condition that occurs when cholesterol and scar tissue buildup, forming a substance called plaque, which narrows and clogs the arteries and slows blood flow to the legs. Since plaque blocks the smaller leg arteries first, PAD is considered a red flag for several life-threatening vascular diseases, such as heart attack (the number one killer in the United States) and stroke. More than 50 percent of PAD patients are asymptomatic and cannot feel the classic warning sign of PAD—leg pain that occurs when walking or exercising and disappears when the person stops the activity. This symptom is typically dismissed as a sign of getting older, as is numbness and tingling in the lower legs and feet, coldness in the lower legs and feet, and ulcers or sores on the legs or feet that don't heal.
In many cases, PAD can be treated with medication (such as blood thinners or drugs that dilate an affected artery), lifestyle changes (such as smoking cessation), diet and a structured exercise program. With early detection, patients could see an interventional radiologist when intervention is most effective and less invasive treatments are still an option. If needed, interventional radiologists can perform minimally invasive angioplasty (the widening of a narrowed or obstructed blood vessel) and/or stenting (the insertion of a tiny mesh tube) to open a blocked artery in the leg and restore blood flow.
A recent study in the Journal of Vascular and Interventional Radiology noted that after a percutaneous vascular intervention (a medical procedure where vascular access is done via needle puncture, rather than by using an open surgical approach) is used to treat PAD, exercise can play an important role in recovery, health and well-being.
"We designed our study to determine whether a percutaneous vascular intervention combined with supplemental supervised exercise therapy is more effective than the intervention alone in improving walking ability in patients with peripheral arterial disease," said Joep A.W. Teijink, M.D., Ph.D., department of vascular surgery, Catharina Hospital, Eindhoven, the Netherlands. The trial evaluated individuals with peripheral arterial disease, all of whom were treated with a percutaneous vascular intervention for an atherosclerotic lesion (a kind of deposit consisting of fat, cholesterol and chalk on the inside of the blood vessels that carry blood away from the heart to the limbs, causing them to become narrowed or blocked).
"Our experience with our research group revealed that the ability to achieve a better walking distance correlates significantly with an individual's quality of life. So at six months after intervention, a treadmill test was used to evaluate 61 individuals who were available for follow-up, on their absolute claudication distance, which is the distance at which the patient experiences pain with exertion to the point that he or she cannot continue walking," said Teijink. "In the group of 34 that had the intervention and additional exercise therapy, 11 were able to go the distance." Teijink concluded, "These significant results reinforced our theory that a solid program of follow-up exercise provides additional health benefits."
Advertisement