Caregivers of patients at home who survived a prolonged critical illness may experience an increased rates of depression finds a new study.
‘Two hundred and eighty caregivers were found to experience high and persistent rates of depression for a year. In order to provide some relief to these caregivers, hospitalists should be attentive to factors associated with caregiver vulnerability and offer support.’





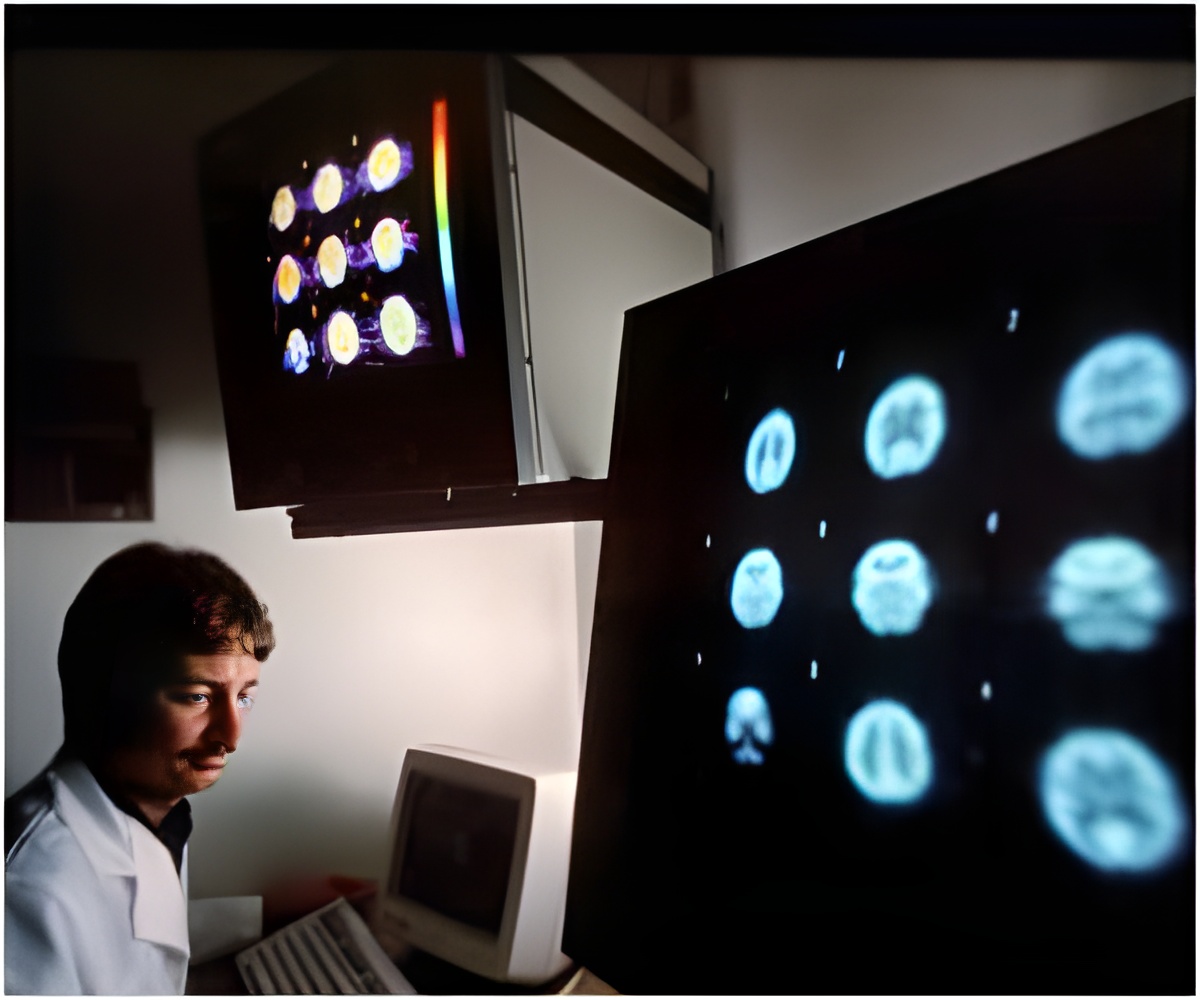
Dr. Ansari was part of a nationwide panel of leading palliative care experts who reviewed and ranked 55 studies about hospital palliative care published in 2016. Palliative care treats pain and other symptoms of serious illness, with the goal of improving quality of life for the patient and family.From the list, the panel selected the nine most significant studies, based on scientific rigor, relevance to hospital medicine and impact on clinical practice.
Here are the studies'findings:
Caregiver depression: More than half of patients with prolonged critical illnesses need support from a caregiver a year after hospitalization. A study that followed 280 caregivers for a year found that many experienced high and persistent rates of depression.
"Hospitalists should be attentive to factors associated with caregiver vulnerability and offer support," Dr. Ansari and colleagues wrote. "Improving caregivers' sense of control and social support may be targets for intervention."
Advertisement
Moral distress among doctors: Moral distress occurs when a clinician feels powerless to take what he or she believes to be the ethically correct action. A study of resident physicians found they experience significant moral distress with futile treatments, such as feeding tubes for patients with advanced dementia. Many said they felt obligated to provide end-of-life care that was not in the patient's best interest and caused the patient to suffer.
Advertisement
Treating cancer pain: One study found that low-dose morphine was superior to weak opioids such as codeine and tramadol for treating moderate cancer pain. Another study found that methadone used as an adjunct pain medication can improve moderate cancer pain.
Inappropriate use of antimicrobials: When a patient is nearing the end of life, a physician may write a comfort care order, which is meant to ensure that the final hours or days are tranquil and pain-free, without prolonging life. But a study found that among 711 patients still alive 24 hours after a comfort care order was written, 15.6 percent still were receiving antimicrobials (antibiotics or antifungals).
Educational videos effective: Advance care planning is making decisions about the care you would wish to receive if you became incapacitated. A study found that using educational videos increased the percentage of hospital patients who did advance care planning.
Palliative care consultations: A study examined the effectiveness of an intervention program for family members of patients with prolonged critical illnesses. The intervention included supportive conversations and information about the illness and prognosis. The team met with family members seven days after the patient went on a ventilator and again 10 days later.
The study found that family members who received the interventions had similar rates of anxiety and depression and higher rates of post-traumatic stress disorder than family members who did not receive the interventions. The study did not evaluate routine specialty palliative care consultation in the ICU. Also, the palliative intervention used in the study was more informational, rather than driven by clinical considerations as in standard consultations.
Source-Eurekalert












