A new, less invasive way to perform transcatheter aortic valve replacement has been developed by researchers at the National Institutes of Health (NIH).

‘A new, less invasive way to perform transcatheter aortic valve replacement has been developed by National Institutes of Health (NIH).
’





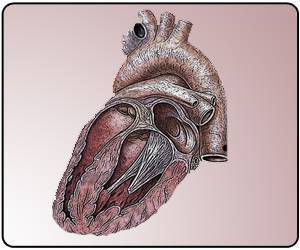
A new, less invasive way to perform transcatheter aortic valve replacement has been developed by researchers at the National Institutes of Health (NIH). The new approach, called transcaval access, will make TAVR more available to high risk patients, especially women, whose femoral arteries are too small or diseased to withstand the standard procedure.
The Journal of the American College of Cardiology published the findings.
Transcaval access, which can be performed in awake patients, involves electrifying a small wire so that it crosses between neighboring blood vessels in the abdomen. The technique calls for making large holes in both the abdominal aorta and the inferior vena cava, which physicians previously considered dangerous because of the risk of fatal bleeding.
The new method was developed by researchers at the National, Heart, Lung and Blood Institute (NHLBI) and tested in a trial on 100 patients at 20 hospitals across the United States. Researchers said it proved successful in 99 of the patients.
Advertisement
Robert J. Lederman, a senior investigator in NHLBI's Division of Intramural Research who led the study, said researchers developed the method to address a specific clinical need, even though they knew it would be a challenging proposition for most surgeons and physicians to accept. The proposed and counterintuitive mechanism of action is that bleeding from the aorta spontaneously decompresses into a corresponding hole the physician makes in the vein, because the surrounding area behind the peritoneum has higher pressure than the vein.
Advertisement
The study builds on the access technique that Lederman's NHLBI team developed and first tested in animals in 2012 and first applied with Henry Ford physicians to help patients in 2013. NHLBI and its collaborators are now working to find ways to train more specialists to perform the procedure.
Source-Eurekalert