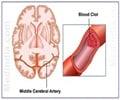
Researchers have developed a new way through which the risk of serious adverse events following ruptured brain aneurysm in stroke patients can be detected.

Comparing 89 patient cases retrospectively, the team found that automated features of existing ICU data were as effective as the transcranial doppler procedure currently used to detect a dangerous constriction of blood vessels in the brain. Transcranial doppler tests require a skilled technician to be available and are often only conducted once a day, and while the test is selective and accurately detects people who are risk, it is not as efficient (sensitivity of 56%) at ruling out which patients are not at greater risk of this serious adverse event .
"There is a great opportunity to utilize abundant existing data to provide guidance and clinical decision support, as this model was as effective and much less resource-intensive," said senior author Soojin Park, MD, assistant professor of Neurology at Penn. "However, while this simple method may be valuable, most ICUs don't have the IT infrastructure to synergize data in such a way."
The team plans to look at prospective cases to compare this method directly with other assessments and clinical decisions.
This study is one of a dozen Penn Medicine studies and talks being presented at the Neurocritical Care Society Annual Meeting. In addition to studies being presented on cerebral blood flow and end of life care in the Neuro Intensive Care Unit, Penn experts are also leading talks on traumatic brain injury, airway management and therapeutic temperature management. Monisha Kumar, MD, assistant professor of Neurology, is also serving on the Society's consensus conference on multimodal monitoring.
Penn's Neurocritical Care Division, formally established in 2004 and led by Joshua Levine, MD, associate professor of Neurology, cares for patients while training the next generation of experts. The program has the second largest number of fellows training in neurocritical care in the United States. In the Hospital of the University of Pennsylvania's Neurocritical Care Unit, a Level I Trauma Center and Acute Brain Injury Center, the team works within one of the most technologically sophisticated neurocritical care units in the nation, the only academic facility of its kind in the region.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4.3 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 16 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $398 million awarded in the 2012 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania - recognized as one of the nation's top "Honor Roll" hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; Chester County Hospital; Penn Wissahickon Hospice; and Pennsylvania Hospital - the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Chestnut Hill Hospital and Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2012, Penn Medicine provided $827 million to benefit our community.
Advertisement