Risk of osteoporosis is higher in postmenopausal women (above 55 years) and requires proper care and monitoring to increase bone density to reduce fractures.

‘Osteoporosis treatment that is stable and has higher bone mineral density with no evidence of new fractures or fracture progression is defined successful.’





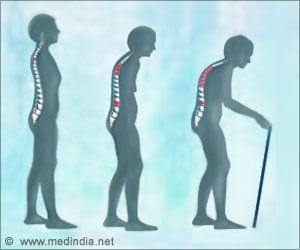
Dr. Camacho is president of the AACE, director of Loyola Medicine's Osteoporosis and Metabolic Bone Disease Center and a professor in the division of endocrinology of Loyola University Chicago Stritch School of Medicine. Osteoporosis is a silent skeletal disorder characterized by compromised bone strength that increases the risk of fracture. Bone strength has two main features: bone density and bone quality.
The guidelines' recommendations are graded from A to D. Most recommendations, including the recommendation to evaluate all women 50 and older, are graded B, meaning they are based on at least one well-designed study.
Recommendations with an A grade are based on the most convincing evidence from multiple gold-standard clinical trials.
A-grade recommendations include:
- Provide counseling on reducing risk of falls, particularly among the elderly.
- Strongly recommend medications for patients with osteopenia or low bone mass and a history of a fragility fracture of the hip or spine. (Osteopenia refers to bone density that is lower than normal peak density but not low enough to be classified as osteoporosis. A fragility fracture is a fracture that results from a fall from a standing height or less).
- Medications that reduce the risk of fractures include alendronate (Fosamax®), risedronate (Actonel®), zoledronic acid (Zometa®) and denosumab (Prolia® and Xgeva®).
- Treatment with teriparatide (Forteo®) should be limited to two years.
Advertisement
Patients at higher fracture risk should continue oral therapy for up to 10 years and IV therapy for up to six years. During the drug holiday in these higher fracture risk patients, another drug such as raloxifene or teriparatide could be considered.
Advertisement
More than two million osteoporosis-related fractures occur annually in the United States, and more than 70 percent of these occur in women.
Among women aged 55 and older, the annual cost of caring for osteoporotic fractures exceeds the annual costs of caring for breast cancer, heart attacks and strokes.
"Despite these significant costs, fewer than 1 in 4 women aged 67 years or older with an osteoporosis-related fracture undergoes bone density measurement or begins osteoporosis treatment," the guidelines state.
Risk factors for osteoporosis include age 65 or older, low body weight, family history of osteoporosis or fractures, smoking, early menopause and excessive alcohol intake (three or more drinks per day).
"Further study is needed to determine the most effective means of communicating benefit and risk in osteoporosis management," the guidelines state. "The best available evidence at this time suggests that communication skills can be learned, decision aids may be helpful and that shared decision-making may improve clinical outcomes."
Source-Eurekalert