The need for transplantable stem cells is great for patients suffering from blood diseases such as leukemia, lymphomas, multiple myeloma and immune deficiency.
‘A precursor cell in the placenta and embryo of mice can be matured in the lab to make hematopoietic stem cells (HSPCs).’





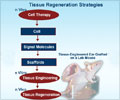
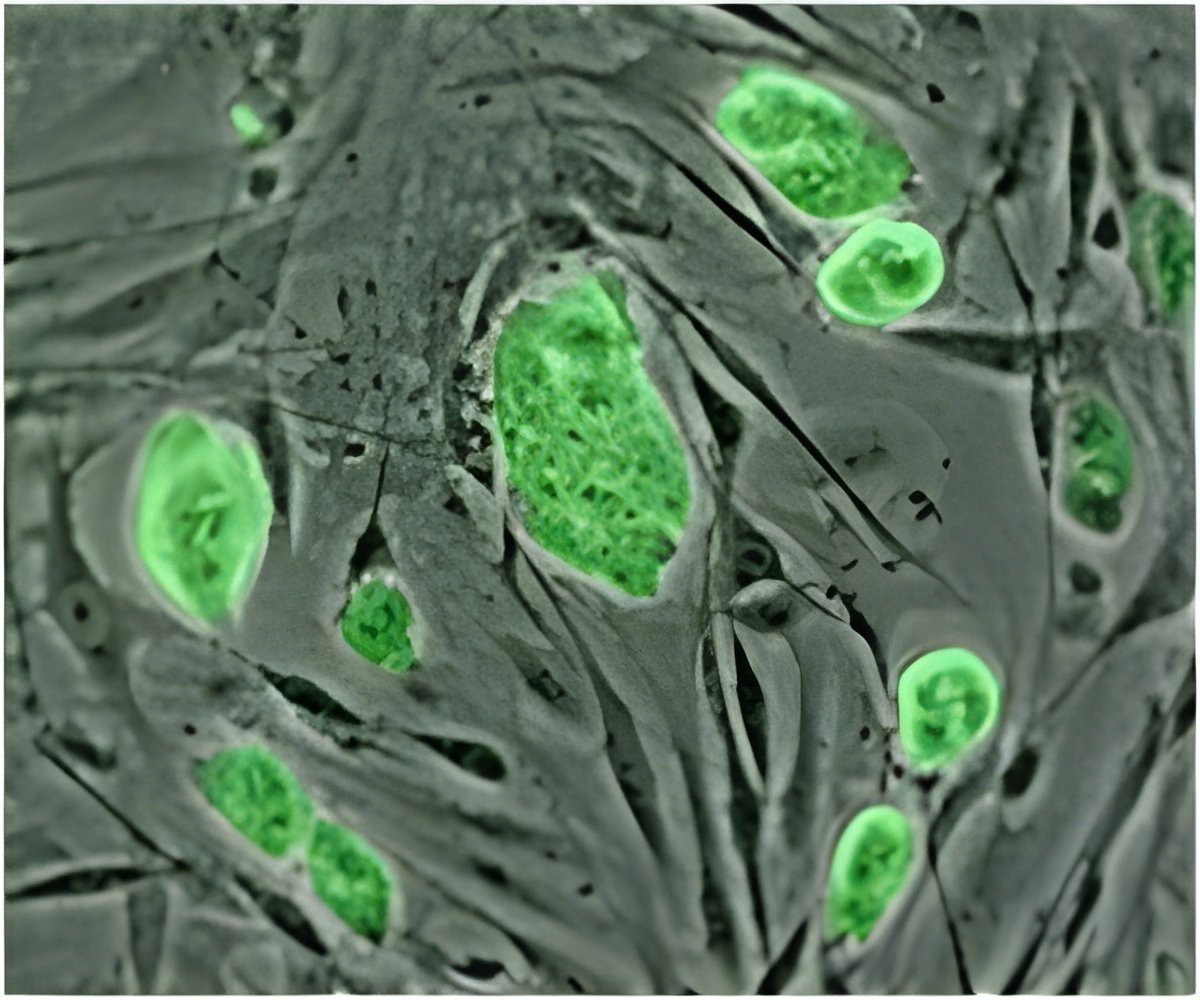
The need for transplantable stem cells is great for patients suffering from blood diseases such as leukemia, lymphomas, multiple myeloma and immune deficiency. Researchers are looking at ways to produce large numbers of HSPCs in the laboratory and developing methods for growing patient-specific HSPCs. The reprogramming process developed by researchers at Icahn School of Medicine at Mount Sinai appears to mimic normal blood cell creation or developmental hematopoiesis -- going from precursor cells to cells that eventually become HSPCs. This technology could potentially provide a different source of stem cells and alleviate this problem. The team analyzed mouse placentas and embryos for the presence of cells with the same phenotype as the precursor cells, and confirmed that they could be matured to HSPCs in the lab.
"To cure disease in the long-term, we need to be able to transplant something that can keep producing new blood cells and won't be rejected by the patient's body," said the senior author of the study, Kateri Moore, DVM, Associate Professor of Developmental and Regenerative Biology at the Icahn School of Medicine at Mount Sinai. "We are excited by the results of our study. The precursor cells can be matured in the lab to transplantable HSPCs. Our reprogramming process can inform developmental hematopoiesis and vice versa."
Other members of the research team included Ihor R. Lemischka, Professor of Developmental and Regenerative Biology, Pharmacology and Systems Therapeutics and member of The Black Family Stem Cell Institute and first author Carlos-Filipe Pereira, former Postdoctoral Fellow of Developmental and Regenerative Biology at the Icahn School of Medicine at Mount Sinai, currently an Assistant Professor at the University of Coimbra, Portugal, Cell Institute.
"Direct reprogramming studies can improve applications for regenerative medicine," said Dr. Lemischka. "Many investigators have attempted to do what we have been able to do growing HSPCs in vitro, but we been able to build upon this process that could move the field forward. The next step is to test these findings in humans."
Advertisement
Advertisement