Scientists at NYU Langone Medical Center conclude new drug in development may offer first alternative to standard chemotherapy for T-Cell Acute Lymphoblastic Leukemia.
An estimated quarter of the 500 U.S. adolescents and young adults diagnosed each year with this aggressive disease fail to respond to standard chemotherapy drugs that target cancer cells.
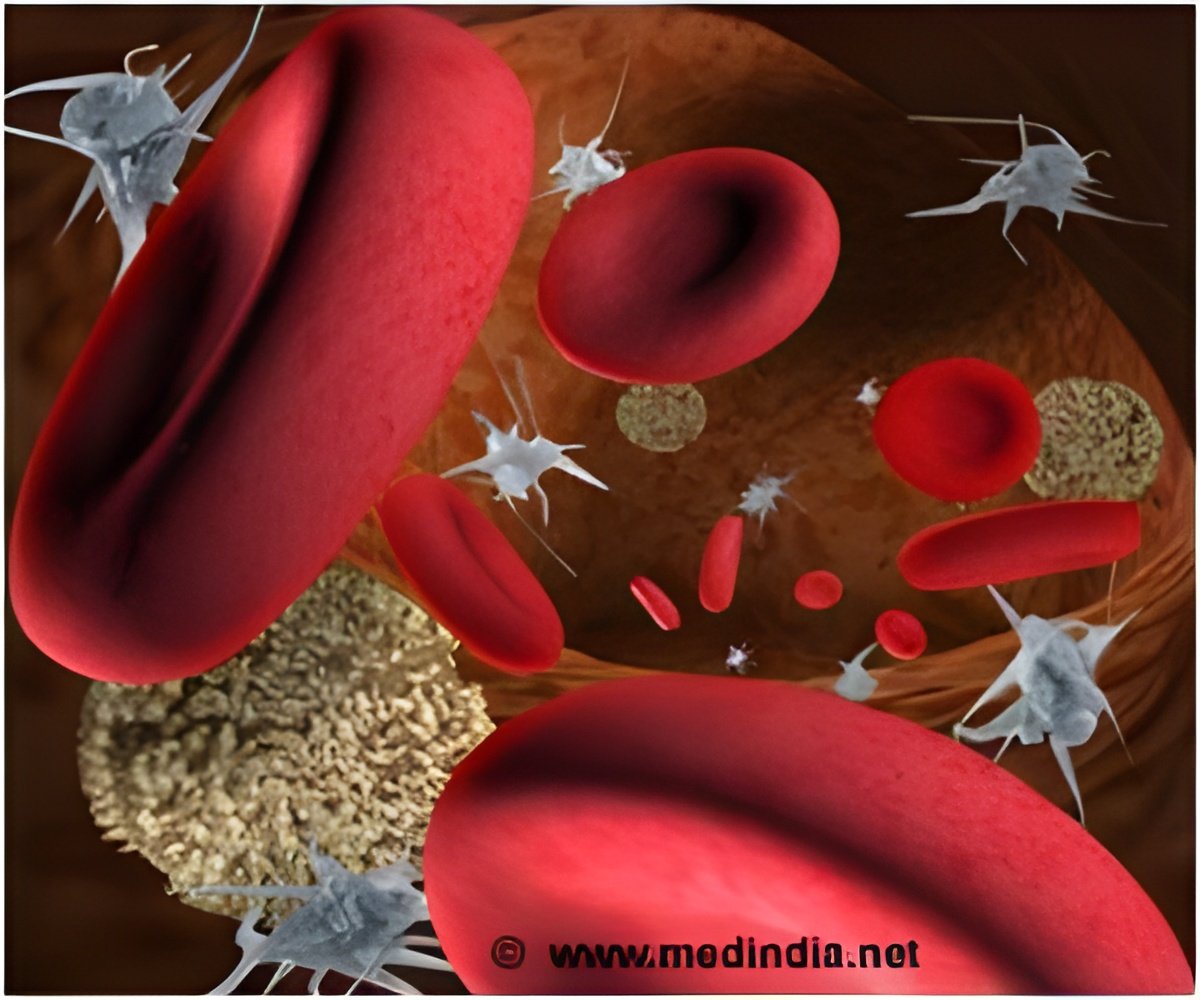
In a report on the work conducted with mice and human laboratory cells, and published in the Oct. 23 edition of the journal Nature, the NYU Langone team concludes that the enzyme JMJD3 -- (pronounced ju-mon-ji D3) -- acts as a cancer "on" switch by splitting off a chemical methyl group of another protein that is usually methylated by a tumor-suppressing enzyme. This enzyme, known as polycomb repressive complex 2 (PRC2), acts, in turn, as an "off" switch for cancer cell proliferation.
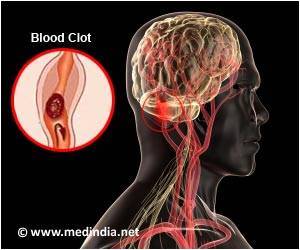
It is this destabilizing and cutting loose of PRC2, the same researchers previously showed, that leads to the activation of the NOTCH1 biological pathway – a process common to many cancers but especially active in at least half of all people with T-cell acute lymphoblastic leukemia.
"Our investigations are showing incredible promise in fighting this disease at the transcriptional level," says senior study investigator and NYU Langone cancer biologist Iannis Aifantis, PhD. "We are blocking the action of enzymes controlling the transcription of proteins involved in leukemia rather than attempting to directly suppress cancer genes."
Advertisement
"Revealing the actions of JMJD3, and successfully blocking the enzyme to stall tumor progression, shows that new treatments for T-cell acute lymphoblastic leukemia are not simply theoretical, but practical," adds Aifantis, chair of the Department of Pathology at NYU Langone and its Laura and Isaac Perlmutter Cancer Center, and an early career scientist at the Howard Hughes Medical Institute.
Advertisement
Specifically, they focused on a protein controlled and methylated by PRC2 called histone 3 lysine 27 (H3K27) as well as two other enzymes closely tied to H3K27 -- JMJD3, and UTX, the latter short for ubiquitously transcribed tetratricopeptide repeat X-linked protein. What the study found is that JMJD3 was highly active in both mice and human leukemia cells at all stages of tumor growth and development. By contrast, UTX was not overly produced in leukemia, but highly active in noncancerous mouse and human cells. When mice and human leukemia cells were treated with the experimental drug GSKJ4, JMJD3 activity stopped and all cancer cells eventually died, the researchers report.
Subsequent genetic experiments showed that in leukemic mice bred so they are unable to make JMJD3, NOTCH1 activity declined, while UTX activity remained the same. The disease also progressed much faster, they found, in mice bred without UTX, while mice lived longer if they produced UTX. The findings suggest that UTX production controls several tumor-suppressing genes.
To further confirm their findings, researchers screened more than 200 blood samples from children and adults with T-cell acute lymphoblastic leukemia, revealing several common mutations in UTX.
Plans are underway, Aifantis says, to test GSKJ4 against human leukemia cells transplanted into mice. Other experiments will use the drug molecule in combination with standard chemotherapy in animals with leukemia.
"Our report serves as a valuable reminder of just how complex cancers like T-cell acute lymphoblastic leukemia can be, and that enzymes can play many, even opposing, roles in both tumor growth and suppression," says Aifantis.
Source-Eurekalert