Inflammation in patients with multiple sclerosis (MS) can be reduced with induced neural stem cells (iNSCs), i.e., by using a patient's own skin cell and re-programming them back to neural stem cells.

‘Personalized stem cell treatment can reduce neuroinflammation in patients with multiple sclerosis (MS).’





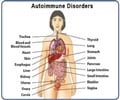
In MS, the body's own immune system attacks and damages myelin, the protective sheath around nerve fibers, causing disruption to messages sent around the brain and spinal cord. Symptoms are unpredictable and include problems with mobility and balance, pain, and severe fatigue.Key immune cells involved in causing this damage are macrophages (literally 'big eaters'), which ordinarily serve to attack and rid the body of unwanted intruders.
A particular type of macrophage known as microglia are found throughout the brain and spinal cord in progressive forms of MS, they attack the CNS, causing chronic inflammation and damage to nerve cells.
Recent advances have raised expectations that diseases of the CNS may be improved by the use of stem cell therapies. Stem cells are the body's 'master cells', which can develop into almost any type of cell within the body.
Previous work from the Cambridge team has shown that transplanting neural stem cells (NSCs) stem cells that are part-way to developing into nerve cells reduces inflammation and can help the injured CNS heal.
Advertisement
A possible solution to this problem would be the use of so-called 'induced neural stem cells (iNSCs)' these cells can be generated by taking an adult's skin cells and 're-programming' them back to become neural stem cells. As these iNSCs would be the patient's own, they are less likely to trigger an immune response.
Advertisement
Using mice that had been manipulated to develop MS, the researchers discovered that chronic MS leads to significantly increased levels of succinate, a small metabolite that sends signals to macrophages and microglia, tricking them into causing inflammation, but only in cerebrospinal fluid, not in the peripheral blood.
Transplanting NSCs and iNSCs directly into the cerebrospinal fluid reduces the amount of succinate, reprogramming the macrophages and microglia in essence, turning 'bad' immune cells 'good'. This leads to a decrease in inflammation and subsequent secondary damage to the brain and spinal cord.
"Our mouse study suggests that using a patient's reprogrammed cells could provide a route to personalized treatment of chronic inflammatory diseases, including progressive forms of MS," says Dr Stefano Pluchino, lead author of the study from the Department of Clinical Neurosciences at the University of Cambridge.
"This is particularly promising as these cells should be more readily obtainable than conventional neural stem cells and would not carry the risk of an adverse immune response."
The research team was led by Dr Pluchino, together with Dr Christian Frezza from the MRC Cancer Unit at the University of Cambridge, and brought together researchers from several university departments.
Dr Luca Peruzzotti-Jametti, the first author of the study and a Wellcome Trust Research Training Fellow, says: "We made this discovery by bringing together researchers from diverse fields including regenerative medicine, cancer, mitochondrial biology, inflammation and stroke and cellular reprogramming. Without this multidisciplinary collaboration, many of these insights would not have been possible."
Source-Eurekalert