Third edition treatment guidelines seek to improve mortality rates for severe pediatric TBI.
‘Severe traumatic brain injury results in approximately 7,000 childhood deaths annually, while survivors of the condition may suffer from long-term health conditions such as seizures, learning difficulty and communication disorders.’





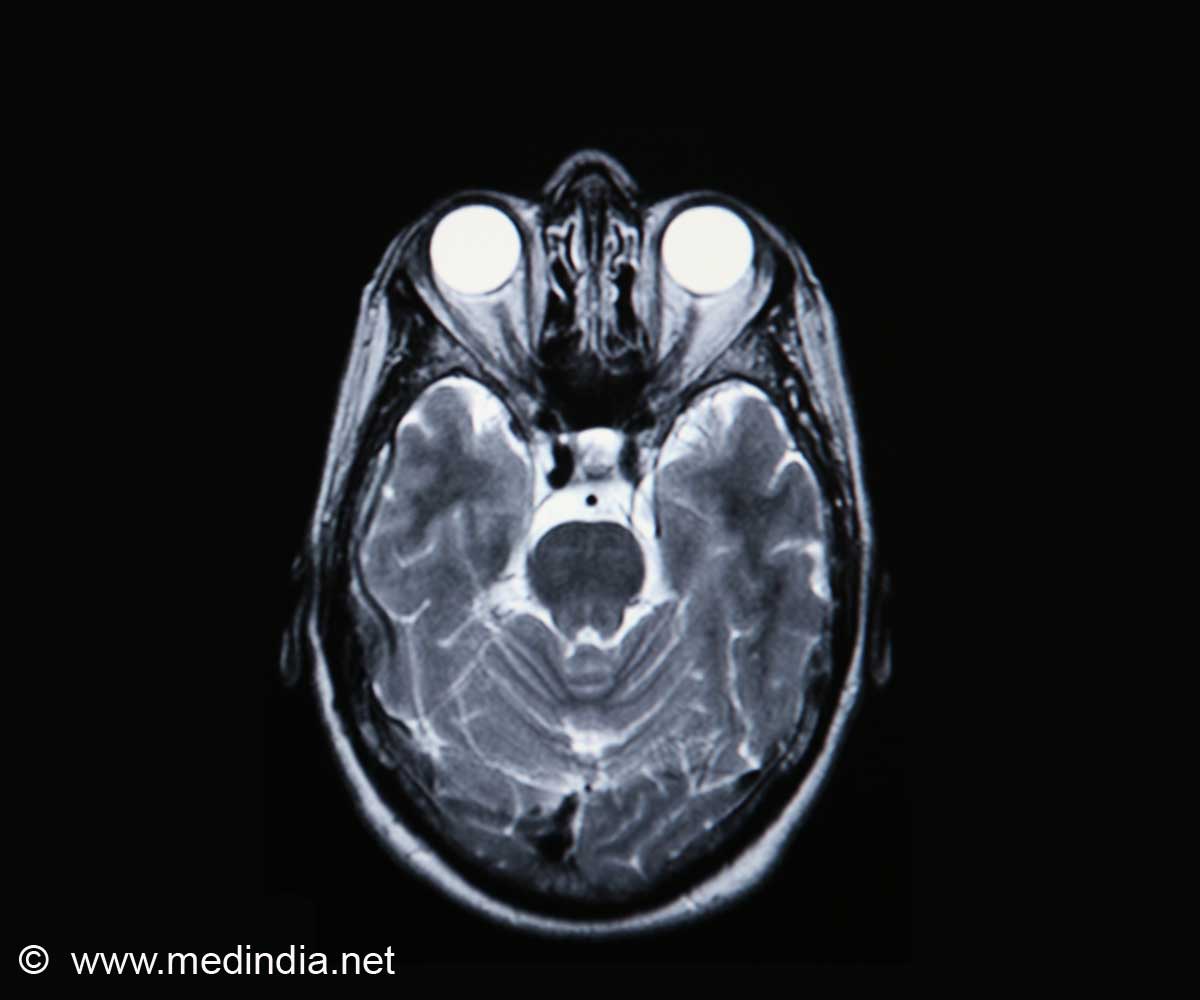
To help promote the highest standards of care, and improve the overall rates of survival and recovery following TBI, a panel of pediatric critical care, neurosurgery and other pediatric experts today issued the 3rd edition of the Brain Trauma Foundation Guidelines for the Management of Pediatric Severe TBI. The updated guidelines reflect the addition of nearly 50 research studies, and include eight new, or revised, treatment recommendations for health care providers that range from the use of intracranial monitoring to the use of hypertonic saline to reduce acute brain swelling.
An executive summary of the guidelines published in the journals Pediatric Critical Care Medicine and Neurosurgery; the full guidelines are available via Pediatric Critical Care Medicine, an official journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
"These guidelines are vital to the proper care and treatment of children with serious brain injury," said co-author and clinical investigator Nathan Selden, M.D., Ph.D., Campagna Professor and Chair of the Department of Neurological Surgery at the OHSU School of Medicine in Portland, Oregon. "Now, health care providers around the world will have access to the best medical evidence and recommendations to help save and improve countless lives."
An associated manuscript, also published in Pediatric Critical Care Medicine, describes an algorithm designed to guide first and second tier therapies for infants and children with severe TBI. The tool for bedside use by caregivers, which supplements evidence-based recommendations in the updated guidelines, was created using a validated, consensus-based expert opinion process. "We believe a combination of research findings and real-life experience will further advance the bedside care of infants and children with severe TBI, especially in treatment scenarios where scientific and clinical research is lacking," said first author Patrick Kochanek, M.D., Grenvik Professor and Vice Chairman of Critical Care Medicine and Director of the Safar Center for Resuscitation Research at the University of Pittsburgh. "This algorithm will also help to identify key research priorities to help ensure the ongoing momentum of consistent, high-quality care for patients across the globe."
Advertisement
Source-Eurekalert