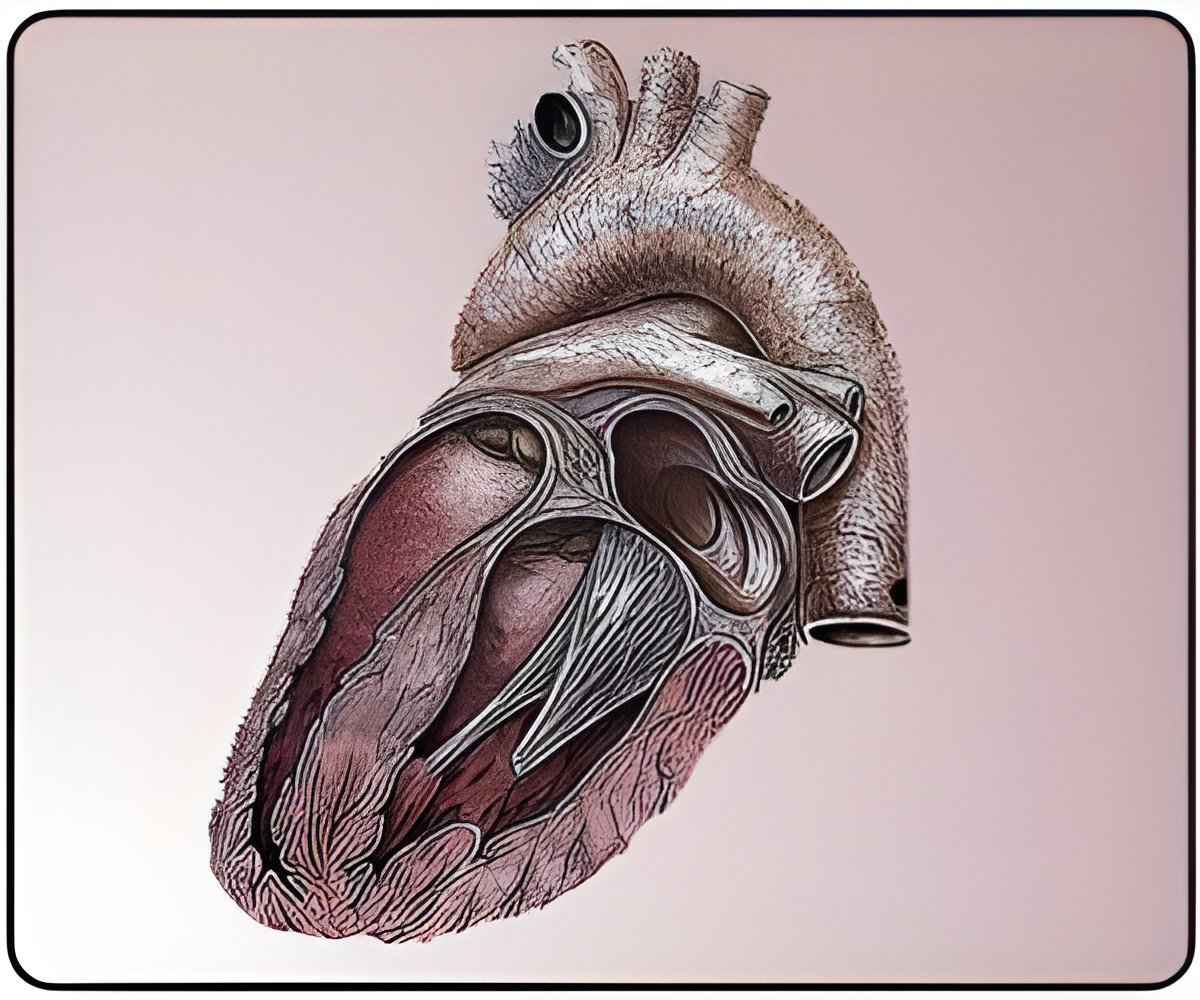
More evidences have now been provided to clarify the role of non alcoholic fatty liver disease as an independent risk factor for the development of cardiovascular disease (CVD)
NAFLD describes a range of conditions where there is a build-up of fat in the liver cells in people who do not drink alcohol excessively. It is rapidly becoming the most common liver disease worldwide, particularly so in the Western world with an estimated prevalence of 20 – 30%. In many cases, NAFLD is linked to being obese or overweight.
Presenting the results of these two studies, EASL's Educational Councillor Professor Jean-Francois Dufour of the University Clinic for Visceral Surgery and Medicine, University of Bern, Switzerland said: "We now have a strong body of evidence that NAFLD may pose a CVD risk above and beyond that conferred by traditional CVD risk factors, such as dyslipidemia, diabetes and smoking. This means that healthcare providers managing patients with NAFLD should take this factor into account in the CVD risk stratification, although the best way to implement this remains to be defined," he added.
NAFLD an early independent predictor of carotid atherosclerotic disease
In a long-term study, patients with NAFLD had a higher prevalence of carotid plaques (44 vs. 37%; p< 0.001), a higher carotid intima-media thickness (C-IMT) (0.64±0.14 vs. 0.61±0.13; p< 0.001), and a higher Framingham score, which measured their 10-year CVD risk (15±9% vs. 8±7%; p< 0.001).
The presence of NAFLD also predicted whether that patient had thickening of the carotid intima-media (beta=0.037; p=0.005), and evidence of early carotid plaques (OR=1.21; 95%CI: 1.03-1.42; p=0.02), independently of the patients' age, sex, BMI, hypertension and tobacco use.
Advertisement
"Whether NAFLD is incidentally or causally associated to early carotid atherosclerosis has previously been the subject of much debate," said Professor Dufour. "While there are case-control studies that have demonstrated a significant and independent relationship between NAFLD and carotid atherosclerotic disease, up until now, long-term follow-up data have been missing."
Advertisement
The Fatty Liver Index (FLI), a surrogate marker of hepatic steatosis when ≥60 years old, and the Framingham cardiovascular risk score (FRS) were calculated.
5,671 patients underwent at least one C-IMT measurement: 52% males; mean age 52±11years; mean BMI = 26.1±4.7; 33% NAFLD; 39% CP, mean C-IMT 0.62±0.13mm. 1,872 patients had 2 C-IMT measurements.
During the 8±4 year follow-up, NAFLD occurred in 12% and carotid plaques in 22% of the patients.
Improvement of NAFLD is associated with a reduced risk of developing DM
A 10-year longitudinal study has confirmed that NAFLD is a significant risk factor for the development of diabetes, and improvement of NAFLD through treatment is associated with a reduced risk of developing diabetes (in submission).
In this study of 3,074 Japanese patients, 117 participants (16.1%) in the NAFLD group developed diabetes during a 10 year follow-up period, compared to only 72 participants (3.1%) in the non-NAFLD group (p< 0.001). The multivariate odds ratio was 2.82 (95% confidence interval: 1.91-4.15) in the NAFLD group compared to the non-NAFLD group.
Moreover, 7 participants (6.4%) in the improved group developed diabetes compared to 110 participants (17.8%) in the non-improved group. In the improved group, the multivariate odds ratio was 0.30 (95% CI: 0.13-0.66), in comparison to the non-improved group.
"Evidence from previous longitudinal studies has demonstrated a clear link between NAFLD and the development of DM," said Professor Dufour. "However, this is the first study to show that DM can be prevented if NAFLD is improved," he explained.
"A multidisciplinary approach is therefore required in the treatment of NAFLD patients, taking into account the presence of NAFLD as a critical part of diabetes prevention and care. New clinical trials to investigate the beneficial effects of anti-diabetes drugs on NAFLD histology, and the potential impact of anti-diabetes drugs on diabetes incidence and cardiovascular risk in non-diabetic patients with early-stage NAFLD are now underway," Professor Dufour concluded.
8,070 participants who had a health check twice between 2000 and 2012 with 10 years between each check were enrolled into this study. An inclusion criterion included having had abdominal ultrasounds during the first and second visits. Exclusion criteria included alcohol use ≧20g/day, positive HBs antigen, positive HCV antibody, and diabetes mellitus at baseline.
The 3,074 eligible participants were divided into the NAFLD group (n=728) and non-NAFLD group (n=2,346), according to ultrasonography-detected fatty liver.
The NAFLD group was then further categorised into the improved group (n=110) and non-improved group (n=618), based on fatty liver disappearance at the second health check. Multivariate odds ratios for the development of DM were estimated by a logistic regression model.
Source-Eurekalert