Preliminary results of a clinical trial in Australia indicate that a noninvasive optical imaging device developed at Cedars-Sinai can provide early detection.

"In preliminary results in 40 patients, the test could differentiate between Alzheimer's disease and non-Alzheimer's disease with 100 percent sensitivity and 80.6 percent specificity, meaning that all people with the disease tested positive and most of the people without the disease tested negative. The optical imaging exam appears to detect changes that occur 15-20 years before clinical diagnosis. It's a practical exam that could allow testing of new therapies at an earlier stage, increasing our chances of altering the course of Alzheimer's disease," said Shaun Frost, a biomedical scientist and the study manager at the Commonwealth Scientific and Industrial Research Organisation. CSIRO is Australia's national science agency.
Frost, first author of the AAIC 2014 abstract, will make the oral presentation. He said 120 participants of a full study of 200 had completed testing.
Keith Black, MD, professor and chair of Cedars-Sinai's Department of Neurosurgery, director of the Maxine Dunitz Neurosurgical Institute and the Ruth and Lawrence Harvey Chair in Neuroscience, said the accumulation of beta-amyloid plaque in the brain is a hallmark sign of Alzheimer's, but current tests detect changes only after the disease has advanced to late stages. Researchers believe that as treatment options improve, early detection will be critical, but existing diagnostic methods are inconvenient, costly and impractical for routine screening.
"PET scans require the use of radioactive tracers, and cerebrospinal fluid analysis requires that patients undergo invasive and often painful lumbar punctures, but neither approach is quite feasible, especially for patients in the earlier stages of disease," he said. Positron emission tomography, or PET, is the current diagnostic standard.
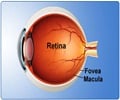
"The retina, unlike other structures of the eye, is part of the central nervous system, sharing many characteristics of the brain. A few years ago, we discovered at Cedars-Sinai that the plaques associated with Alzheimer's disease occur not only in the brain but also in the retina. By 'staining' the plaque with curcumin, a component of the common spice turmeric, we could detect it in the retina even before it began to accumulate in the brain. The device we developed enables us to look through the eye – just as an ophthalmologist looks through the eye to diagnose retinal disease – and see these changes."
Advertisement
The retinal beta-amyloid plaque findings and optical imaging technology began at Cedars-Sinai with studies in live rodents and the post-mortem investigation of human retinas of people who had died with Alzheimer's. Maya Koronyo-Hamaoui, PhD, assistant professor of neurosurgery in the Department of Neurosurgery and the Department of Biomedical Sciences, and Yosef Koronyo, a research scientist, were first authors of the original results that were published in a journal and presented at the AAIC in 2010. The Australian study is one of several in progress to determine if similar results can be confirmed in humans living with the disease.
Advertisement
Source-Eurekalert