One of the most common causes of mortality in intensive care units worldwide is severe sepsis, which is a disease characterised by a sudden drop in blood pressure

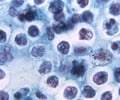
In most cases, severe sepsis is triggered by an infection, that is, the invasion of our body by a microbe (pathogen). The disease is known to develop from an uncontrolled reaction against the infectious agent, rather than by the infectious agent itself. Through a series of experiments conducted in mice, Miguel Soares and colleagues found that hemoglobin is the unusual suspect behind this uncontrolled reaction. Hemoglobin is normally enclosed inside red blood cells where it carries oxygen. It associates with four other molecules, called heme groups, each containing an iron atom that binds oxygen. During sepsis, however, hemoglobin is released from red blood cells (a process called hemolysis) and looses its heme groups that become toxic. These can cause cells in several organs to die, lead to the dysfunction of multiple organs and eventually death.
Rasmus Larsen, first author of this study, explains, "We first demonstrated a role for heme in worsening organ injury during sepsis. We found that as heme accumulates in the blood, the levels of a hemopexin, a molecule that neutralises the toxic effects of free heme, decreases, suggesting a way to control the harmful effects of free heme. We started a very productive collaboration with Ann Smith (University of Missouri, USA) that had been working with hemopexin for many years. She sent us enough of this protein that we could administer it to mice after they started developing severe sepsis. We found that when we did this the general health status of these animals improved markedly, with the majority of them surviving the infection, as compared to the non-treated mice that died."’
The team took their research a step further: in collaboration with Fernando Bozza at the Fundação Oswaldo Cruz in Rio de Janeiro, Brazil, they showed that amongst infected patients diagnosed with septic shock in the intensive care unit, those that died had lower levels of circulating hemopoxin in the blood, as compared to those that survived, confirming the observations made in mice by Rasmus Larsen at the IGC. Miguel Soares and Rasmus Larsen explain, "These observations suggest that hemopoxin may be used as a predictor of mortality in patients developing severe sepsis: if levels are too low, we can expect a more severe outcome of the disease, and possible death".
These findings may lead to a new approach to treat severe sepsis. Miguel Soares continues, "While many drugs are efficient in killing the pathogen that triggers severe sepsis, on its own this approach is not sufficient to prevent mortality. By administering hemopexin, which provides protection against organ destruction, we open the way for an alternative way to treat sepsis (aside from killing the pathogen) that may potentially save the lives of thousands of patients in intensive care units worldwide."
Advertisement