Chimeric antigen receptor (CAR) T-cell therapies utilize a patient's own T cells that have been genetically engineered to bind to a specific antigen on target cancer cells.
‘CAR-Ts are living cellular biologics—genetically reengineered versions of a patient’s own immune cells that have been programmed to recognize and kill cancer cells.’





In addition, when a subcutaneous tumor began to recur two months after CAR T-cell therapy and a surgical biopsy was performed, the CAR T-cells spontaneously re-expanded and the tumor again went into remission, and phenomenon that had not previously been reported. While the patient eventually relapsed and died more than a year after CAR T-cell therapy, the brain tumor never recurred. "Brain involvement in DLBCL carries a grave prognosis, and the ability to induce a complete and durable response with conventional therapies is rare," explains Jeremy Abramson, MD, of the MGH Cancer Center , lead author of the letter in the Aug. 24 NEJM. "In addition, all available CAR T-cell trials have excluded patients with central nervous system involvement. This result has implications not only for secondary DLBCL like this case but also for primary central nervous system lymphoma, for which treatment options are similarly limited after relapse and few patents are cured.
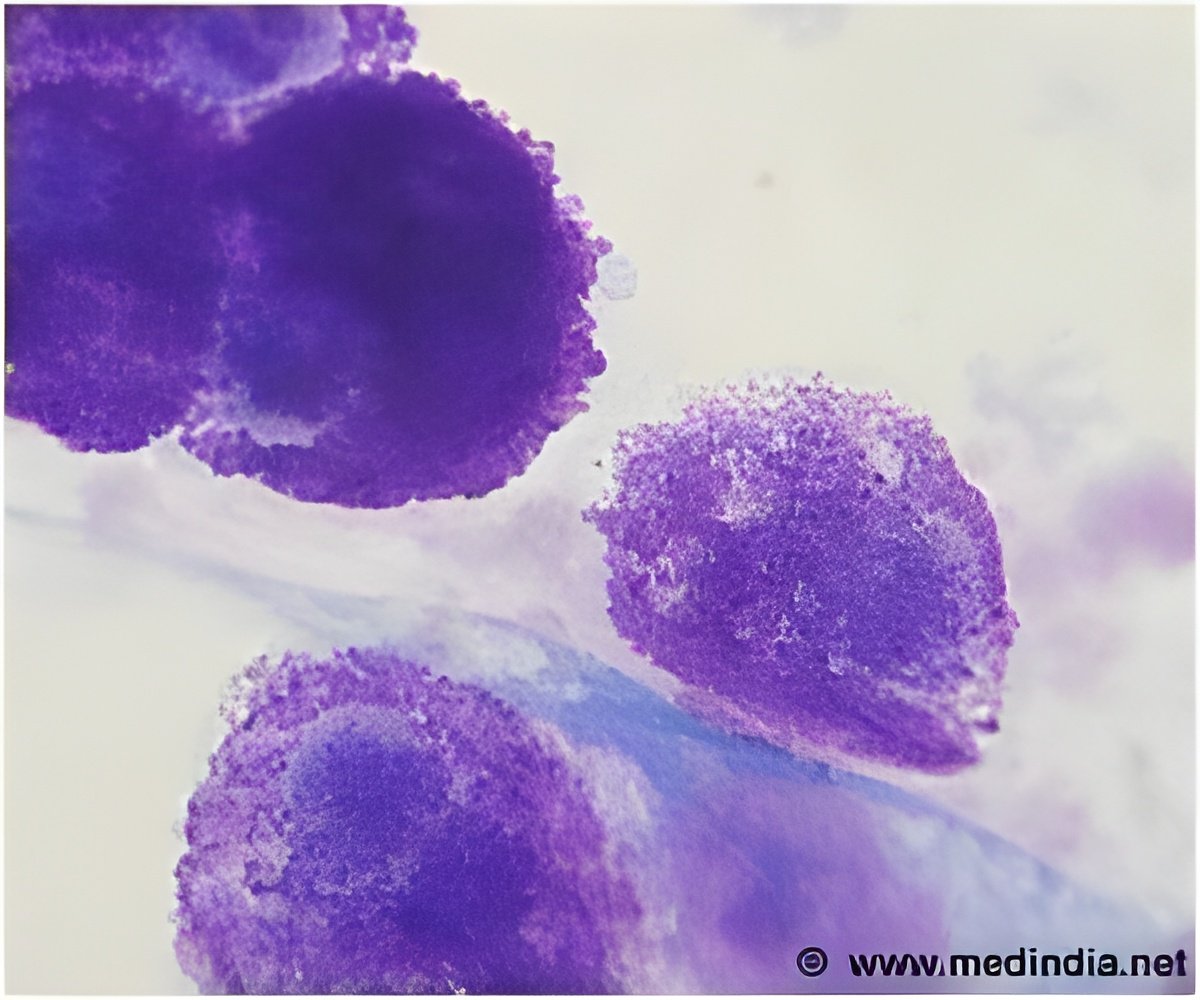
CAR T-cell therapies utilize a patient's own T cells that have been genetically engineered to bind to a specific antigen on target cancer cells. This clinical trial sponsored by Juno Therapeutics is testing JCAR017, which targets the CD19 protein expressed on most B-cell leukemias and lymphomas. The most common type of non-Hodgkin lymphoma in adults, DLBCL is an aggressive cancer that can develop in many types of tissue.
This patient was a 68-year-old woman with DLBCL that had not responded either to conventional chemotherapies or to a stem-cell transplant, a situation that usually leads to a life expectancy of less than six months. After enrolling in the study -- a phase 1 trial designed to investigate the safety and antitumor activity of JCAR017 - -she was found to have new lesion in the right temporal lobe of her brain.
One month after the study treatment -- which involves chemotherapy followed by intravenous infusion of JCAR017 -- follow-up imaging showed complete remission of the brain lesion. The subcutaneous lesion that recurred two months later disappeared after the biopsy with no further treatment. Blood testing showed an expansion in the numbers of CD19-targeted CAR T-cells that coincided with the tumor's regression. While re-expansion of CAR T-cells has been reported in response to other immunotherapy drugs, this is the first report of such a response to a biopsy.
Advertisement
Source-Eurekalert