A novel mechanism, similar to how normal tissue stem cells respond to wounding, may explain why bladder cancer stem cells contribute to chemo-resistance after multiple cycles of chemotherapy drug treatment.
The results of their study appear online in the journal Nature today.
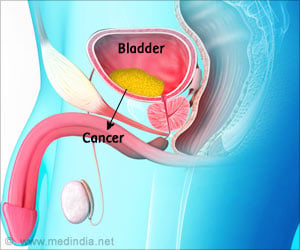
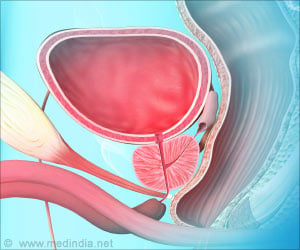
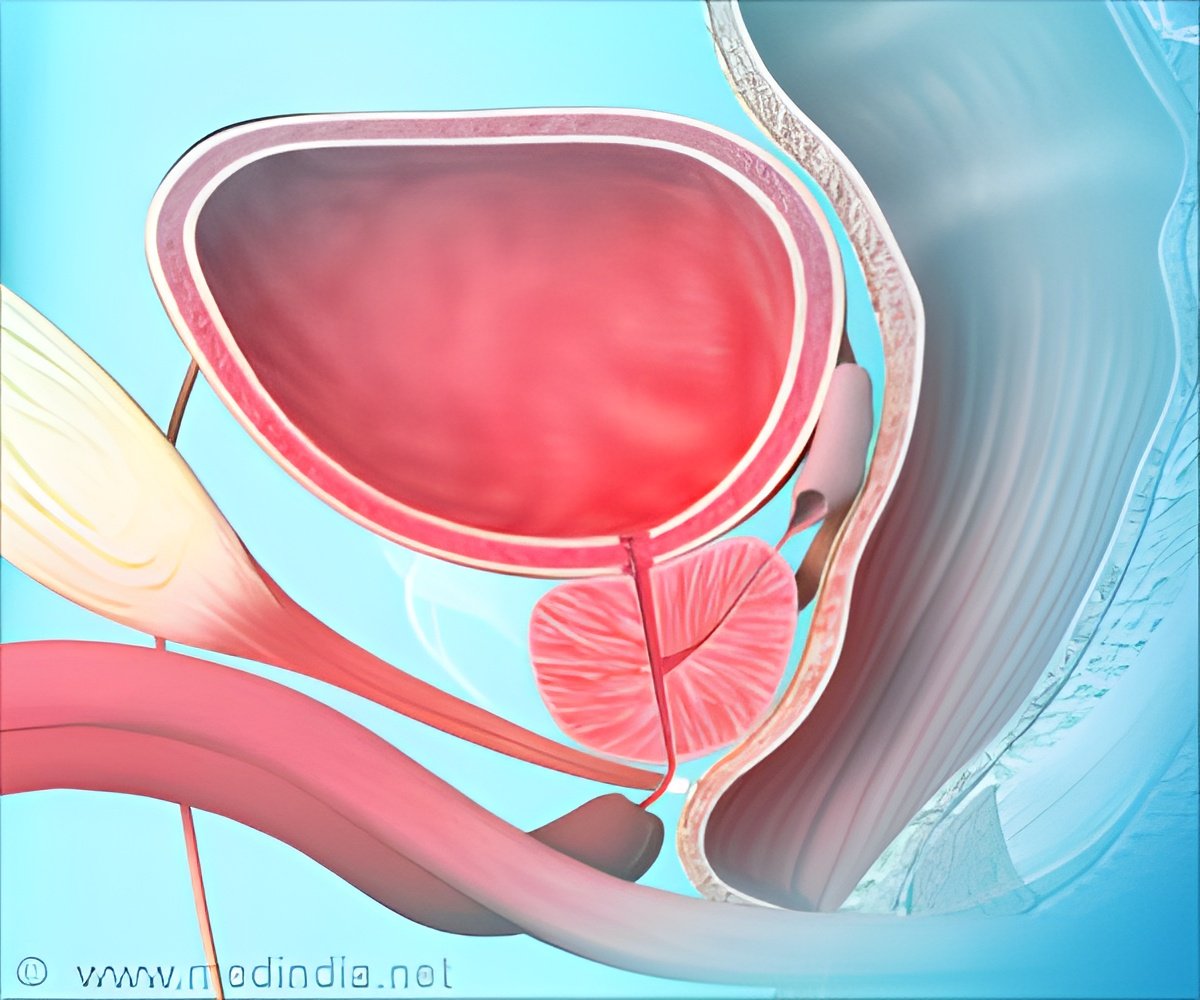
"Treatment for advanced bladder cancer is limited to surgery and chemotherapy. There are no targeted treatments available," said Dr. Keith Syson Chan, an assistant professor of molecular and cellular biology and of urology and the corresponding author on the report. "The chemotherapy response is far from ideal so the clinical goal is to advance research into this area and uncover a much more targeted approach."
Together with co-lead authors Antonina Kurtova, a graduate student in the Translational Biology and Molecular Medicine Program at Baylor, and Dr. Jing Xiao, research assistant in urology at Baylor, Chan and his team sought out to identify mechanisms underlying the development of resistance in bladder cancer that has invaded the muscles. They found that regrowth of cancer stem cells actively contributes to therapy resistance between drug treatment cycles.
"This is a paradoxical mechanism leading to resistance, one we didn't expect," said Chan. "The cancer stem cells actively regrow and respond to the induced damage or apoptosis (cell death) caused by chemotherapy in between the different cycles, similar to how normal tissue stem cells respond to wound-induced damages."
The proliferation is stimulated by the release of a metabolite (or factor) called prostaglandin E2 or PGE2 from the dying cells, which causes the cancer stem cells to repopulate tumors that were reduced in size by chemotherapy, they found.
Advertisement
Chan said it is important to note that chemotherapy is administered in multiple cycles, which actually evokes the surprising finding.
Advertisement
"What would happen if you block PGE2?" the researchers asked.
In studies conducted in mice, the team found that blocking PGE2 abolished the induction of "wound-response" that fuels the regrowth of the cancer stem cells.
In one mouse experiment using tumors extracted from a human patient who previously failed chemotherapy, the team observed an enhanced therapeutic response.
"Importantly, we were able to use a drug already approved by the U.S. Food and Drug Administration," said Kurtova. "This should help us quickly speed up time to start of human clinical trials."
That drug was Celecoxib or Celebrex®, a drug most commonly used as a treatment for arthritis.
Further study in clinical trials is necessary, but the study provides a promising new find in a type of cancer with no current targeted options, Chan said. Importantly, this treatment may be applicable to other types of solid cancers, he said.
Source-Eurekalert