Explore the elevated risk of stillbirth in pregnancies complicated by obesity, especially as term approaches.
- Maternal obesity significantly increases the risk of stillbirth
- The heightened risk intensifies with gestational age, particularly at term
- Employing a nuanced prenatal counseling approach is essential to counter bias and stigma, fostering positive outcomes for mothers and infants alike
The impact of isolated obesity compared with obesity and other risk factors on risk of stillbirth: a retrospective cohort study
Go to source). In a recent large-scale study published in the Canadian Medical Association Journal (CMAJ), the connection between obesity and an elevated risk of stillbirth during pregnancy has been explored. The study, conducted by lead author Dr. Naila Ramji and her colleagues, sheds light on the nuanced relationship between obesity, gestational age, and stillbirth risk.
The study emphasizes the implications for maternal care and the need for a nuanced approach in prenatal counseling for individuals with obesity.
Obesity: A Growing Concern for Stillbirth Risk
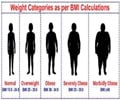
The study, analyzing data from the Better Outcomes Registry and Network on over 681,000 singleton births in Ontario between 2012 and 2018, reveals that obesity significantly increases the risk of stillbirth as pregnancy progresses.While the overall stillbirth rate in Canada is approximately 0.4%, individuals with class I obesity (BMI 30–34.9 kg/m2) have double the risk of stillbirth at 39 weeks gestation compared to those with a normal BMI (18.5–24.9 kg/m2). The risk further escalates for those in obesity classes II and III, reaching 2 to 2.5 times the risk at 36 weeks, and more than fourfold at 40 weeks.
Noteworthy is the comparison with other medical conditions associated with stillbirth, where guidelines recommend delivery at 38 or 39 weeks with lower risk thresholds than those identified for obesity-related risks.
Did You Know?
Obesity is increasing at alarming rates with a current prevalence of more than 42% in US adults and 17% in children. Around 50% of US women of reproductive age (20–39 years) are either overweight (25.6%) or suffer from obesity (24.8%).
Delving Deeper: The Impact of Gestational Age and Obesity Class
The study suggests that pregnant individuals with obesity, particularly those with additional risk factors, may benefit from more vigilant surveillance and timely referral closer to term.The authors propose the consideration of earlier delivery for those with higher classes of obesity and emphasize the importance of addressing implicit biases within the medical community to ensure that the risks associated with obesity are taken seriously.
Furthermore, the researchers discovered a higher risk of stillbirths occurring before delivery in individuals with class I and II obesity, highlighting the need for specialized care for this at-risk population. These findings underscore the necessity of tailoring maternal care strategies to the unique needs of individuals with obesity during pregnancy.
Read More to Know About ‘Maternal Obesity May Harm Mother and Baby’
Beyond Numbers: Addressing Implicit Bias and Stigma
In a related editorial, CMAJ editor Dr. Naomi Cahill emphasizes the importance of a nuanced approach in prenatal counseling for patients with obesity. Dr. Cahill warns against focusing solely on weight during risk communication, as it may reinforce weight bias, stigma, and discrimination.Negative attitudes and stereotypes prevalent in society can lead to adverse physical and mental health consequences for pregnant individuals with obesity.
In conclusion, the study's findings contribute significantly to the understanding of the intricate relationship between obesity and stillbirth risk during pregnancy. The call for a nuanced approach in prenatal counseling aligns with the broader goal of providing respectful care free from stigma, ensuring positive maternal and fetal outcomes for pregnant individuals with obesity.
As we navigate this complex landscape, addressing implicit biases and tailoring care strategies will be crucial in effectively mitigating the risks associated with obesity and improving outcomes for both mothers and their infants.
Reference:
- The impact of isolated obesity compared with obesity and other risk factors on risk of stillbirth: a retrospective cohort study - (https://www.cmaj.ca/content/196/8/E250)
Source-Medindia