New study analyzed the effect of obesity surgery on diabetes remission and the factors that predict it, together with the likelihood of relapse.

‘The risk of microvascular complications was 47% lower in the RYGB group than in the control population, with large decreases in the risk of diabetic retinopathy (48%) and diabetic kidney disease (46%). ’





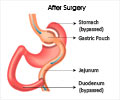
The research, conducted by Dr Lene R Madsen, Professor Bjørn Richelsen and colleagues at Aarhus University Hospital, Aarhus, Denmark, looked into the effects of RYGB surgery on obese (BMI >35 kg/m2) individuals with T2D in a real-world setting. Within the last 20-30 years, bariatric surgery has become a common treatment for obesity in individuals both with and without T2D. Until recently RYGB surgery was the method of choice, especially for individuals with both obesity and T2D, and clinical trials have reported short-term remission of diabetes in around 75-90% of patients.
Predictors for higher likelihood of success include the patient being younger, lower glycated haemoglobin levels (HbA1c, which is an indication of lower blood glucose levels and thus blood sugar control), shorter duration and lesser severity of diabetes, and the individual being male. Emerging long-term follow-up data have also revealed a considerable risk of the disease reappearing after the initial remission period.
This study analysed the effect of RYGB on diabetes remission and the factors that predict it, together with the likelihood of relapse. It also studied the risk of surgical complications, and the incidence of microvascular and macrovascular complications.
The team chose a group of 1111 individuals with T2D who were treated with RYGB surgery in hospitals in Northern Denmark from 2006 to 2015, and compared them with a matched cohort of 1074 patients with T2D who were not operated upon. Diabetes remission was defined as no glucose-lowering drug use along with HbA1c <48 mmol/mol (<6.5%), or metformin monotherapy with HbA1c <42 mmol/mol (<6.0%). Various medical registries were used to obtain data about postoperative complications, and relapse was defined as HbA1c rising to 48 mmol/mol or above, or the patient being prescribed glucose-lowering drugs following an initial discontinuation. The health of participants was followed until the end of the study period (31 December 2015), except in cases where they had left North Denmark or died prior to that date.
Advertisement
The authors note that the strongest predictor of a patient not going into remission was if they required insulin to control their disease. This resulted in a 43% lower remission rate than the average for the cohort. Other factors included age with participants aged 60 or over having a 17% lower remission rate than those under 40, as well as a lower average starting HbA1c level (48 vs 57 mmol/mol). The remission group also had a lower average duration of living with the disease at 2.6 years, compared with 7.0 years for the non-remission group.
Advertisement
Readmission due to surgical complications during the 30 days after RYGB surgery occurred in 7.5% of patients, which the authors point out is "higher than we previously reported among RYGB-operated individuals overall (3.3%), most likely because type 2 diabetes per se disposes to surgical complications." They add, however, that surgical short-term mortality was very low (under 0.5%).
The authors say: "The findings from this study add to the growing body of evidence on effects of bariatric surgery, specifying that RYGB does cause remission of type 2 diabetes and is associated with a reduced risk of microvascular, and possibly macrovascular complications...Predictors of remission success seem to be very consistent in randomised controlled trials, studies of selected cohorts and population-based studies."
They add: "On the other hand, there is a substantial risk of relapsing into type 2 diabetes, which should be accounted for when advising patients and planning post-surgery care."
Source-Eurekalert