A new large-scale international study finds that taking a break from hormone-blocking prostate cancer treatments once the cancer seems to be stabilized is not equivalent to continuing therapy.
But this new study, which treated 1,535 patients with metastatic prostate cancer and followed them for a median of 10 years, finds that's not the case. Results appear in the New England Journal of Medicine.
"We tried to see whether intermittent androgen deprivation is as good as continuous androgen deprivation, but we did not prove that. We found that intermittent therapy is certainly not better and moreover we cannot even call it comparable," says lead study author Maha Hussain, M.D., FACP, a prostate cancer expert oncologist at the University of Michigan Comprehensive Cancer Center.
The study was sponsored by SWOG, a National Cancer Institute-supported cancer clinical trials cooperative group.
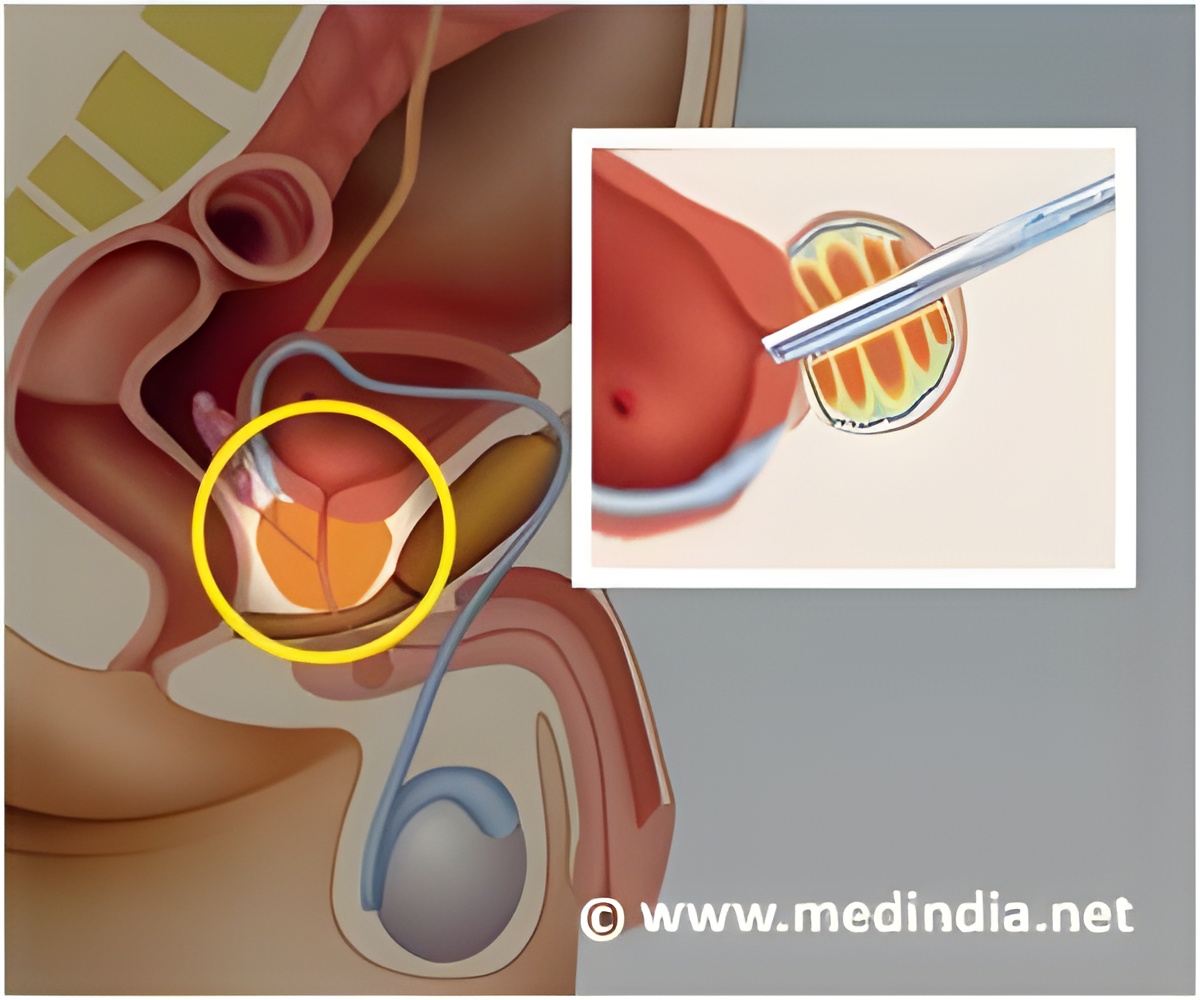
In the study, men with metastatic hormone-sensitive prostate cancer were given an initial course of androgen deprivation therapy (hormone therapy), which is standard therapy for this disease. Patients with a stable or declining PSA level equal to or below a cut-off of 4 ng/ml were then randomly assigned either to continue or to discontinue the hormone therapy. Patients were carefully monitored with monthly PSAs and a doctor's evaluation every three months and therapy was resumed in the intermittent arm when PSA climbed to 20 ng/ml. The intermittent cycle continued on-and-off based on the PSA levels.
Survival among the two groups showed a 10 percent relative increase in the risk of death with intermittent therapy, with average survival of 5.8 years for the continuous group and 5.1 years for the intermittent group from the time of randomization.
Advertisement
"The improvements in some aspects of quality of life that were observed early were not sustained after a few months as patients had to resume therapy," says Hussain professor of internal medicine and urology at the U-M Medical School.
Advertisement
Follow-up studies are investigating a new generation of anti-hormone treatments combined with current therapies in the hopes of increasing the treatment's effectiveness. For information about currently available clinical trials at U-M, call the Cancer AnswerLine at 800-865-1125.
Prostate cancer statistics: 238,590 Americans will be diagnosed with prostate cancer this year and 29,720 will die from the disease, according to the American Cancer Society.
Source-Newswise


![Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis](https://images.medindia.net/patientinfo/120_100/prostate-specific-antigen.jpg)