Spinal surgery for fractures caused by osteoporosis offers no better pain relief than a sham or placebo in older patients reveals result from a trial on older patients with osteoporosis.

‘When compared with pain relief in patients undergoing vertebroplasty (surgery to repair spinal fractures) or a placebo where patients are given local anesthetic injections (but no bone cement), patients who had the spinal surgery did not have better pain relief and there was no improvement on their quality of life or on disability.
’





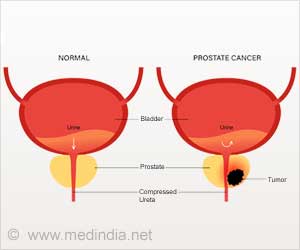
Osteoporosis is a disease in which bones become weak and more likely to break. Fractures caused by osteoporosis most often occur in the spine and are called vertebral compression fractures. Long term, these fractures can lead to deformity, breathing problems, and loss of height. Vertebroplasty involves injecting a special cement into the fractured bone to stabilise it and to relieve pain. But previous studies have reported conflicting results and there is ongoing debate about its benefits, risks, and cost-effectiveness.
To try to resolve this uncertainty, researchers in the Netherlands and the USA compared pain relief in patients undergoing vertebroplasty or a 'sham' procedure, where patients are given local anesthetic injections, but no bone cement.
The trial involved 180 adults aged older than 50 years, with 1-3 painful vertebral compression fractures of up to nine weeks old. Participants were randomly assigned to either vertebroplasty (91 patients) or the sham procedure (89 patients).
The main (primary) outcome measure was mean reduction in pain scores at one day, one week, and one, three, six, and 12 months after the procedure. Other (secondary) outcomes were differences in quality of life and disability over 12 months.
Advertisement
The mean reduction in VAS pain score was statistically significant in both groups at all follow-up points after the procedure, compared with baseline. However, these changes in VAS scores did not differ significantly between the groups over the 12 month follow-up period.
Advertisement
"Percutaneous vertebroplasty to treat patients with acute osteoporotic vertebral compression fractures did not result in statistically significant more pain relief than a sham procedure during 12 months' follow-up," say the researchers.
They point to some study limitations, such as lack of an untreated control group and limited generalisability to other treatments. However, strengths over previous trials included larger patient groups and longer follow-up.
They believe there is a place for vertebroplasty "when efficacy outweighs the risks," but conclude that these results "do not support using percutaneous vertebroplasty as standard pain treatment in patients with acute osteoporotic vertebral compression fractures."
This trial suggests that vertebroplasty "should not be offered to patients with three or fewer painful osteoporotic vertebral fractures of less than 6-9 weeks' duration," says Evan Davies, consultant spinal surgeon at Southampton General Hospital, in a linked editorial.
However, questions remain on its place in the management of chronic painful fractures, and, more specifically, whether cement augmentation has any role in the prevention of long term morbidity and mortality, he adds.
These are fruitful areas for further research, he writes, In the meantime, early vertebroplasty - before nine weeks - "should probably be considered only in exceptional circumstances for patients with vertebral osteoporotic fractures."
Source-Eurekalert