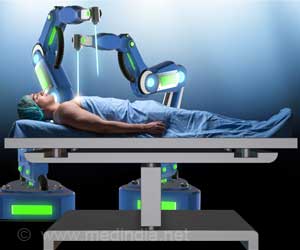
Robotic-assisted surgery vs. laparoscopic surgery for kidney removal or rectal cancer have been compared. No improvements seen in robotic-assisted compared with laparoscopic surgery.
‘Robotic-assisted laparoscopic surgery is very expensive, but does not appear to be beneficial over conventional laparoscopic techniques.’





In one study, In Gab Jeong, M.D., Ph.D., of the Stanford University Medical Center, Stanford, California, and University of Ulsan College of Medicine, Seoul, and colleagues examined the use of robotic-assisted radical nephrectomy (kidney removal) in the United States and compared the in-hospital outcomes and costs between this procedure and laparoscopic radical nephrectomy. The study included patients who had undergone one of these procedures for a renal mass at 416 U.S. hospitals between January 2003 and September 2015.
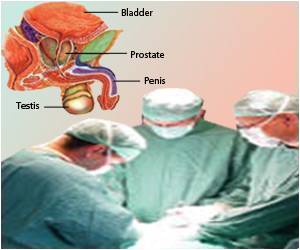
The use of robotic surgery has increased in urological practice over the last decade. However, the use, outcomes, and costs of robotic nephrectomy have not been known.
Among 23,753 patients included in the study, 18,573 underwent laparoscopic radical nephrectomy and 5,180 underwent robotic-assisted radical nephrectomy.
Use of robotic-assisted surgery increased from 1.5 percent (39 of 2,676 radical nephrectomy procedures in 2003) to 27 percent (862 of 3,194 radical nephrectomy procedures) in 2015.
Advertisement
In another study, David Jayne, M.D., of the University of Leeds, United Kingdom, and colleagues compared robotic-assisted vs conventional laparoscopic surgery for risk of conversion (change due to unforeseen complications that arise during surgery) to open laparotomy (surgical incision through the abdominal wall) among patients undergoing resection (surgical removal) for rectal cancer.
Advertisement
The study, conducted at 29 sites in 10 countries, included patients with rectal cancer who were randomized to robotic-assisted (n = 237) or conventional (n = 234) laparoscopic rectal cancer resection.
The overall rate of conversion to open laparotomy was 10.1 percent.
The researchers found that there were no statistically significant differences in the rates of conversion to open laparotomy for robotic-assisted laparoscopic surgery compared with conventional laparoscopic surgery (8.1 percent vs 12.2 percent, respectively), and there were no statistically significant differences in complication rates or quality of life at six months.
"These findings suggest that robotic-assisted laparoscopic surgery, when performed by surgeons with varying experience with robotic surgery, does not confer an advantage in rectal cancer resection," the authors write.
Source-Eurekalert