At UT Southwestern Medical Center, a multidisciplinary team has found that measuring the oxygenation of tumors can be a valuable tool in guiding radiation therapy, opening the door for personalized therapies that keep tumors in check with oxygen enhancement.
Over the past several years, the research of Dr. Mason, professor of radiology and the paper's senior author, and his colleagues has been building on findings that show lack of oxygen actually stimulates the growth of new blood vessels in tumors and leads to metastasis and genetic instability in cancer. The theory follows that breathing oxygen or enriching the oxygen content of hypoxic (low in oxygen) cancer tissues improves therapy.
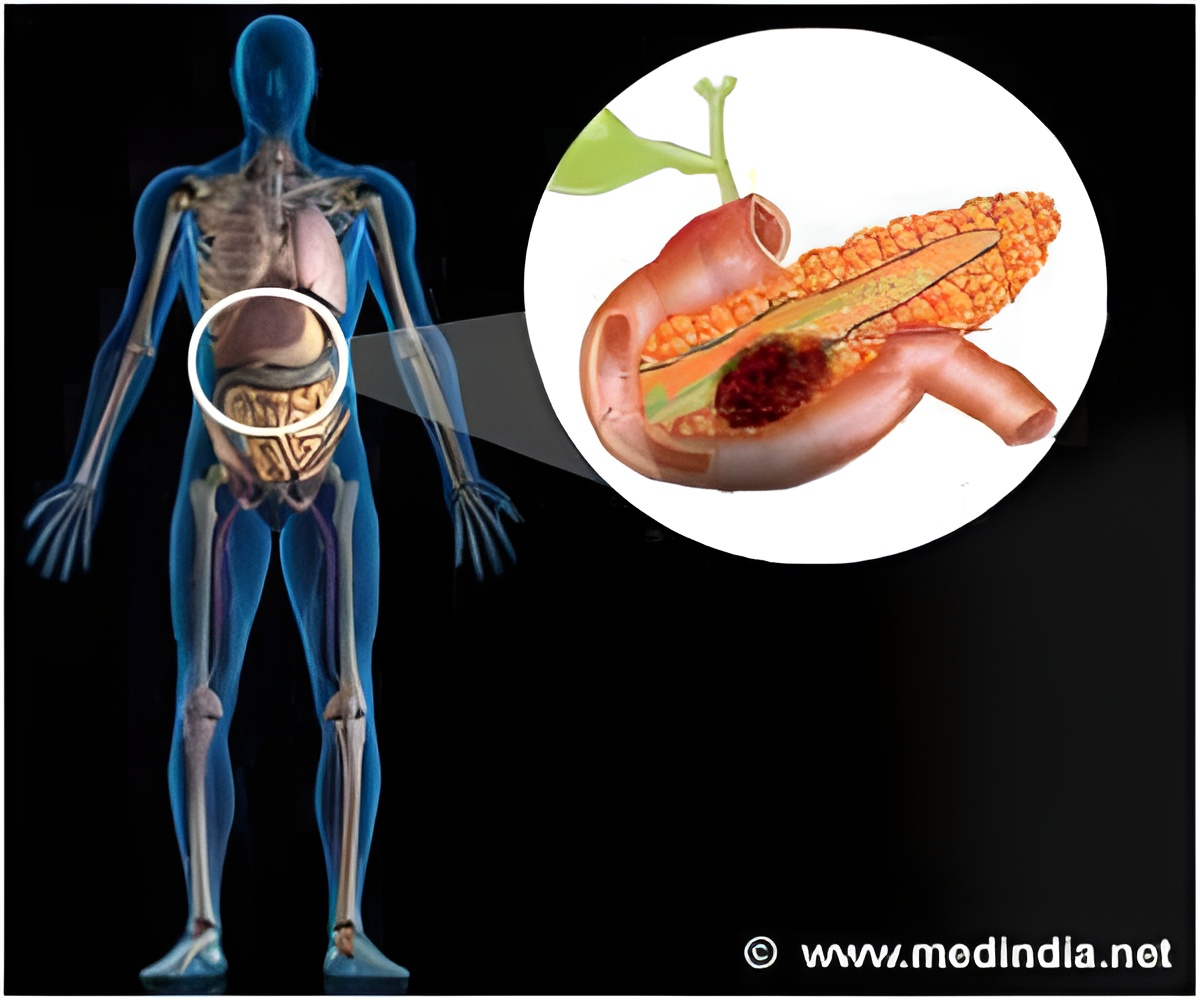
In the current study, supported by the National Cancer Institute, smaller tumors based on magnetic resonance imaging were found to be significantly better oxygenated than larger ones. This confirmed previous investigations that show a range of hypoxic environments depending on the size of the tumor.
"The next step is clinical trials to assess tumor response to radiation therapy," said Dr. Mason, director of the cancer imaging program at the medical center. "Tumors determined to be hypoxic can be evaluated and made responsive through mild and easy-to-administer interventions, such as breathing more oxygen or taking a vasoactive drug. Monitoring the response to oxygen breathing tells us which tumors will benefit."
If the results are confirmed in humans, the implications for personalized therapies for other cancers could mean fewer radiation treatments, or perhaps, ideally, one single high-dose treatment. Lung cancer, for instance, is a form of the disease whose tumors are poorly oxygenated despite being located in the principle organ charged with oxygenating the blood.
"The ability to stratify tumors based on hypoxia offers new opportunities to tailor therapy to tumor characteristics, potentially enhancing success through personalized medicine," Dr. Mason said.
Advertisement
With CPRIT support, Dr. Mason's team has worked to understand how low oxygen concentration can cause radiation resistance in tumors. In some cases, the simple addition of oxygen to stereotactic body radiation greatly improves response. The key is to identify those patients who will benefit.
Advertisement















