Brain imaging using radioactive dye can detect early evidence of Alzheimer's disease that may predict future cognitive decline among adults with mild or no cognitive impairment.

"Our research found that healthy adults and those with mild memory loss who have a positive scan for these plaques have a much faster rate of decline on memory, language and reasoning over three years," said lead author P. Murali Doraiswamy, M.D., professor of psychiatry and director of the neurocognitive disorders program at Duke.
Alzheimer's disease – which currently has no cure – afflicts an estimated five million U.S. adults, and is the sixth-leading cause of death among adults, according to the Centers for Disease Control and Prevention. Prior studies have found that changes in the brain begin years, and possibly decades, before cognitive symptoms emerge.
A biomarker that could accurately identify those at greatest risk for cognitive decline could help clinicians better evaluate and treat patients, while also accelerating the testing of drugs to treat the disease.
The current study, which enrolled 152 adults ages 50 and older, was designed to assess whether silent pathological changes in the brain associated with Alzheimer's and detected with positron emission tomography (PET) can predict cognitive decline. Of the participants, 69 had normal cognitive function at the start of the study, 52 had been recently diagnosed with mild cognitive impairment, and 31 were diagnosed with Alzheimer's disease.
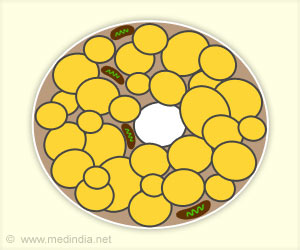
Subjects completed cognitive tests and underwent PET scans of their brains. This type of imaging uses a radioactive tracer to look for chemical signs of disease in specific tissues.
Advertisement
After 36 months, the researchers repeated the same cognitive exams to reassess participants. They found that those with mild or no cognitive impairment who had evidence of plaques at the trial's start worsened to a greater degree on cognitive tests than those with negative scans.
Advertisement
Conversely, those with negative scans experienced much less decline: 90 percent of participants with mild cognitive impairment but no plaque did not progress to Alzheimer's. This finding supports the negative predictive value of using PET imaging to identify patients unlikely to decline, which has important implications for both clinical research and treatment."Having a negative scan could reassure people that they are not likely to be at risk for progression in the near future," Doraiswamy said.
Doraiswamy cautioned that florbetapir is currently not approved to predict the development of dementia and is not used as a screening tool in cognitively normal people. Future longitudinal studies are needed to further clarify the prognostic role of beta-amyloid plaque PET imaging in a clinical setting."Even though our study suggests the test has predictive value in normal adults, we still need additional evidence," Doraiswamy said. "We need longer-term studies to look at the consequences of silent brain plaque build-up, given that it affects 15 to 30 percent of normal older people."
Doraiswamy added that the findings provide support for planned and ongoing multicenter clinical trials of asymptomatic older adults with plaque-positive scans. The research also has implications for other conditions where amyloid might play a role, such as traumatic brain injury (from sports or combat).
Source-Eurekalert