An injury to the anterior cruciate ligament (ACL) is fairly common, especially among young athletes.
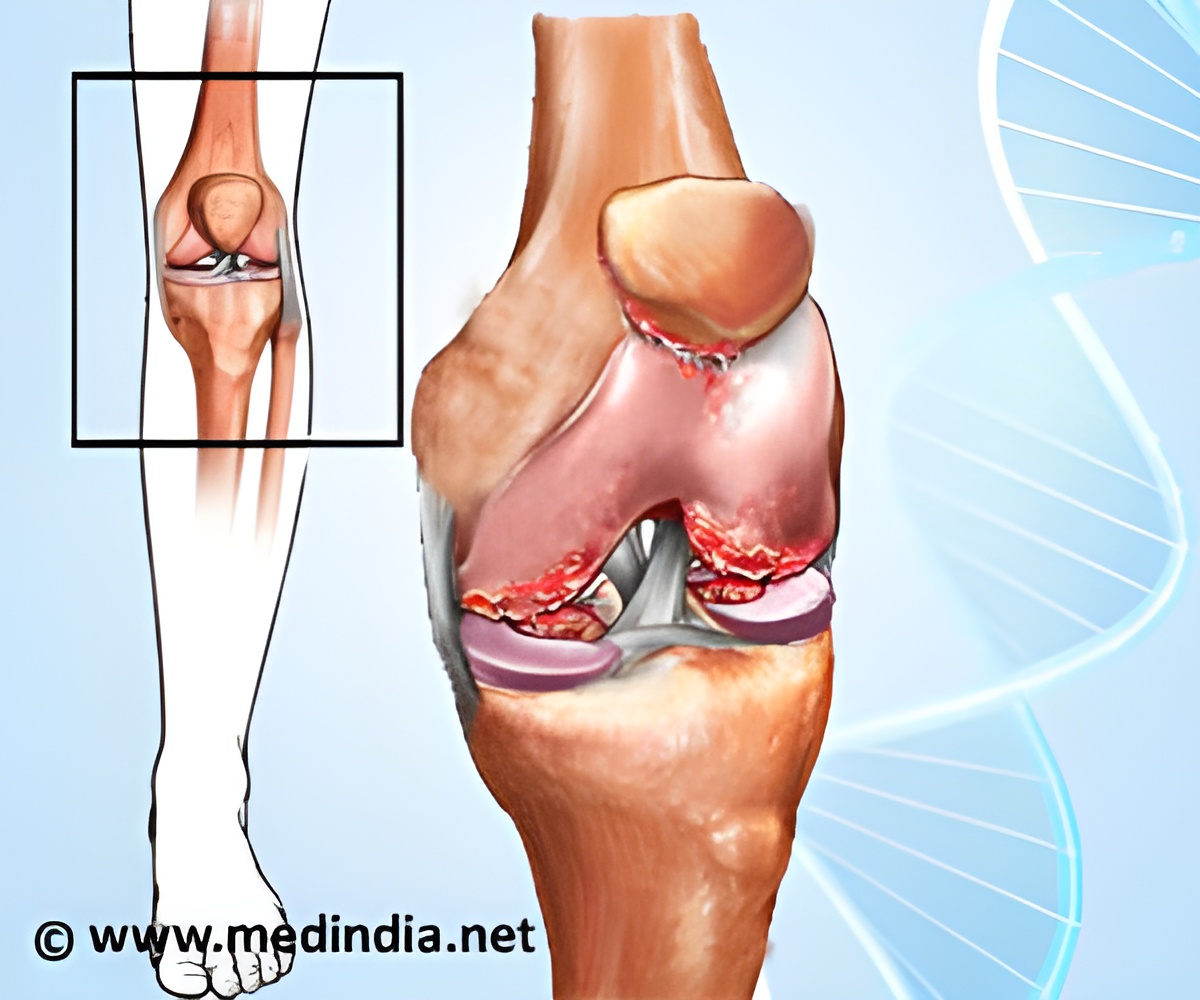
The most movable joints in the body, known as synovial joints, contain synovial fluid (SF). This fluid acts as a lubricant to reduce friction between cartilage in the joint during movement. Following a traumatic injury to the ACL, SF concentration of the natural lubricant, lubricin, in the injured joints is significantly lower in those joints than in the healthy, uninjured joint.
The goal was to identify biologic methods to address the loss of lubricin. In their study, they used animal models with torn ACLs to test three types of fluids that could be injected into the joints and could serve as a substitute for the lost SF. The first was human synoviocyte lubricin that was created in a culture and then purified to be injected into the injured knees. The second is recombinant protein, with a change in the genetic make-up of the cell so that it makes a molecule of interest. The reasoning behind using a recombinant protein is that if it is commercialized, that is likely how it will be manufactured. The third was lubricin from human SF that would otherwise be discarded. The human SF is then purified before injection, and because it is more closely aligned with the natural lubricin, it represents a positive control in the study.
Through their study, the researchers report three key findings. Jay, who is also a professor of emergency medicine and engineering at The Warren Alpert Medical School of Brown University says, "First and foremost, we found that you can limit cartilage deterioration. This is evident by using a well-accepted OA biomarker which shows that the breakdown of cartilage collagen type 2 and recovered in the urine has been muted by treating the knee joint with lubricin." The human synoviocyte lubricin was the most effective form in this experiment, however, the recombinant form also had a good degree of success.
Second, the study results indicate that when lubricin is placed back into the traumatized joint, it encourages the joint to make its own lubricin. Jay explains, "We found that you are limiting deterioration of the joint endogenously by the greater secretion of the lubricin molecule. Basically, by placing the lubricin there, it encouraged the joint's normal activity to produce this molecule."
Jay, who is also a physician with University Emergency Medicine Foundation in Providence, stresses that this study is important for another reason. "This is a huge advance over the existing technology of viscosupplementation injections. The concept was good, but the chemistry isn't there to support it." Jay continues, "When viscosupplements were approved as devices in the 90s, it was thought then that hyaluronic acid used in this treatment was tied to joint lubrication because it was viscous. We now know that joint lubrication has little to do with viscosity. We are inventing a new type of joint lubrication strategy: Tribosupplementation, taken from the Greek, meaning to wear or to rub" "
Advertisement
Jay and his colleagues believe the study findings represent that paradigm shift. Jay says, "We found that lubricin may prevent the fundamental process that can lead to OA following an ACL injury. It is a promising biologic candidate since it is a replacement for a normally occurring glycoprotein. This is very germane to the health care bill, which supports the creation of new therapeutic biologics." Biologics are important and their development is encouraged because they are very specific and have low toxicity profiles, meaning they are better for patients in terms of better results with fewer complications.
Advertisement
Source-Eurekalert