Researchers along with Intel Corp. have collaborated to synthesize and study a grid-like array of short pieces of a disease-associated protein on silicon chips.

"When I see patients in the clinic right now, I may know they have arthritis, but I don't know which of the 20 or 30 types of the disease they have," said associate professor of medicine Paul (P.J.) Utz, MD, noting that existing methods can take days or even weeks to answer such questions. "Now we can measure thousands of protein interactions at a time, integrate this information to diagnose the disease and even determine how severe it may be. We may soon be able to do this routinely while the patient is still in the physician's office."
Utz is a co-senior author of the research, published online Aug. 19 in Nature Medicine. Postdoctoral scholar Chih Long Liu, PhD, and Madoo Varma, PhD, director and head of life science research operations and business strategy for Intel's Integrated Biosystems Laboratory, are the other senior authors. Graduate student Jordan Price is the first author. The research was funded in part by Intel Corp., and Intel scientists created the protein array on the silicon chips for the Stanford researchers to study.
Within each of our cells, proteins enter into and disband physical relationships in dizzying succession — outdoing even our most-freewheeling Facebook friends. This intricate dance forms the machinery responsible for driving cell growth, sparking immune reactions and even causing disease. But understanding the microscopic minutiae of their fleeting attractions (why exactly is protein X hooking up with protein Y?), and the subsequent biological repercussions, has been difficult and time-consuming.
To better understand these interactions, researchers at Intel synthesized short segments of biological proteins, called peptides, on silicon wafers. To do so, they turned to the same process used to make semiconductors, employing a method using sequential steps of light exposure and chemical reactions called photolithography. The Stanford researchers then used the chip, which they've termed an Intel array, to analyze thousands of protein interactions simultaneously to diagnose disease, assess therapies and even design more-effective drugs.
The researchers hope to eventually embed an integrated semiconductor circuit within the microprocessor-ready silicon chip to create a sort of minicomputer that could take the guesswork and decision-making out of many clinical processes. It could perhaps spell out patient-specific diagnoses with letters of the alphabet, or identify which potential treatments are most likely to be effective.
Advertisement
About four years ago, however, researchers at Intel approached Utz and his colleagues with the idea of using silicon as a microarray platform to synthesize the peptides directly on the chip, rather than making the peptides separately and spotting them on the array using a robot.
Advertisement
There's also the promise of devising new, faster detection methods on the more-versatile silicon chip.
"If we couple these Intel arrays with an electronic detection method, for example, we could have real-time sensing over a period of minutes," said Utz.
In the study, the researchers tested whether their array could help categorize patients with lupus — an autoimmune disease in which patients make antibodies that attack a type of protein in their cells called a histone (in addition to other proteins).
"Lupus is highly variable, and in some cases is quite severe," said Utz. "About half of patients are likely to require more intensive therapy. We wanted to see whether we could identify these patients with our arrays."
Using the new silicon chips, the researchers were able to identify patients with lupus who expressed high levels of antibodies against a particular histone called 2B. They then confirmed that these patients were precisely the ones struggling with a more severe form of the disease.
"Companies developing therapies to block the pathway responsible for this binding are now accepting patients with lupus for clinical trials without knowing which subset of disease they are in," said Utz. "This method could potentially be used to identify only those patients likely to benefit, and aid in the identification of effective drugs."
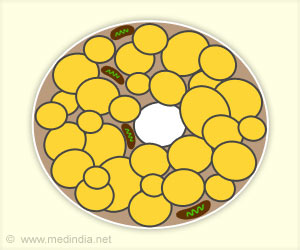
To make the discovery, the researchers made a microarray using the last 21 amino acids of histone 2B. Histones keep DNA packaged tightly within a cell's nucleus; binding of various proteins to the exposed end of the histone selectively grants or excludes access to the packed genes. The global importance of the binding events, and the fact that autoimmune diseases like lupus arise when the body makes antibodies against the histone's end, led the researcher to choose it for their first test of the technology.
In making the array, they synthesized every possible overlapping sequence of every length from the short string of amino acids: 1-21 (the full-length sequence) to 17-20 (four amino acids) to 2-20 (19 amino acids) and all other possible variations. Three of the amino acids are also sometimes modified to carry extra chemical groups that can enhance or impede protein binding. Including every possible length and combination of modified and unmodified amino acids gave nearly 9,000 unique peptide dots on the array. They then washed the chip with solutions of antibodies known to bind the sequence.
The pattern of binding showed that one antibody could recognize and bind to a sequence composed of only two amino acids of the original 21. Another required at least four amino acids, one of them modified, for binding. Analyzing the binding of solutions of other antibodies in each case delineated specific binding regions, or epitopes, within the original short sequence.
Understanding the binding at such levels of detail will allow researchers to tinker with drugs meant to disrupt, enhance or mimic biological reactions within our cells to create better therapies, or to understand how and why natural processes sometimes go awry.
The researchers are now exploring the use of the technique to help design influenza vaccines that elicit a strong immune response, as well as ways to incorporate the three-dimensional folding involved in most protein interactions.
Source-Eurekalert