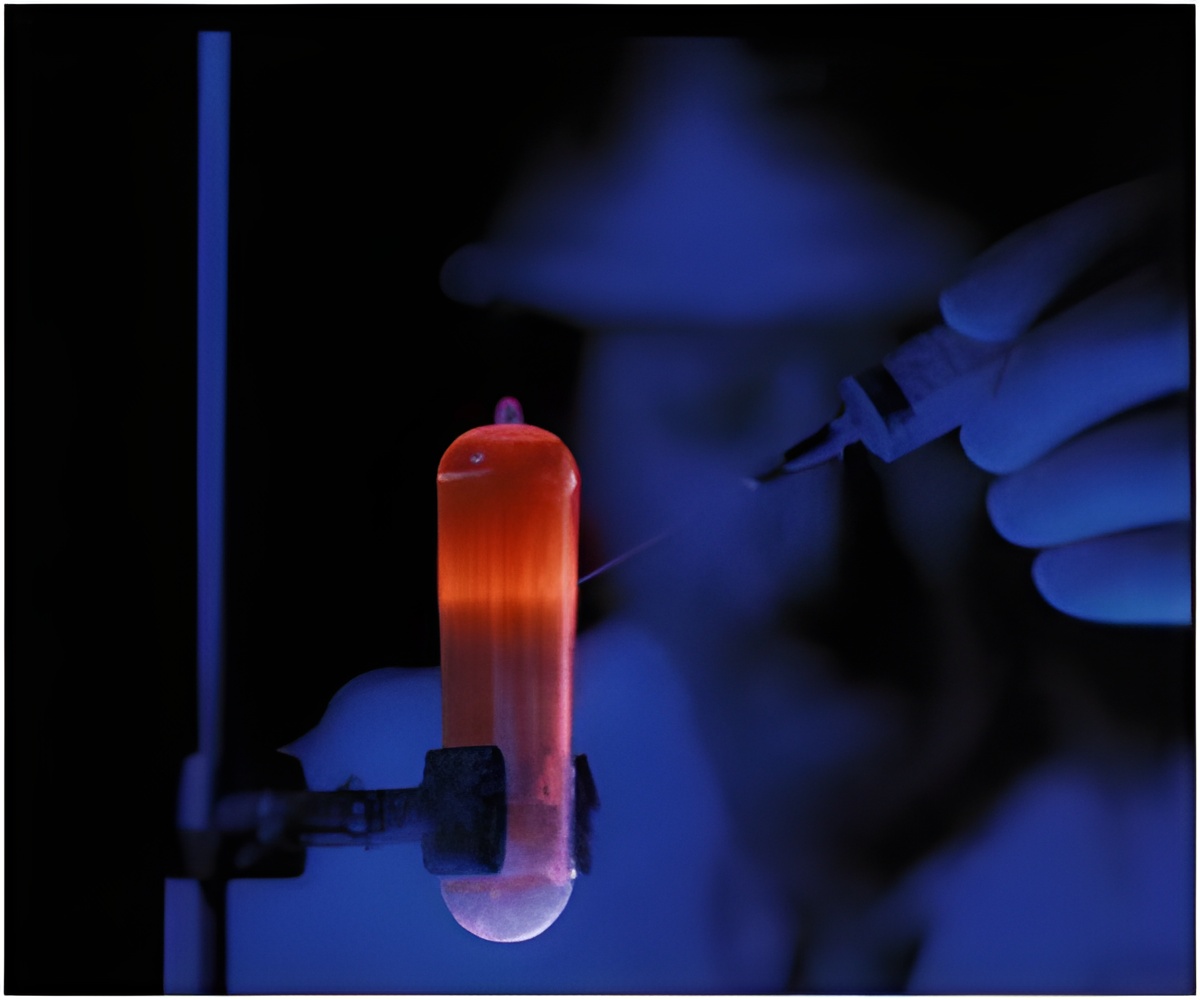
Appendiceal cancer has a distinctive genomic landscape and researchers have developed an organotypic slice culture of living appendiceal cancer cells.
What is Appendiceal Cancer
Appendiceal cancer (malignancies of the appendix, a small tissue pouch that is part of the gastrointestinal tract) is very rare, occurring in perhaps one or two people per 1 million per year. Prognoses is mixed, with a 5-year survival rate of 67 to 97 percent for low-grade tumors detected early, but much lower for advanced cases that may have spread to other parts of the body. For cancer researchers attempting to study appendiceal cancer and find remedies, a primary challenge has been the lack of an effective preclinical model to probe its pathology and test new drugs or therapeutic approaches.‘The organotypic model accurately recapitulates appendiceal tumors in terms of cell mix and behavior, which makes it a promising new research tool in addition to other approaches, such as organoids and patient-derived xenografts (transplanted tissue grown in another species, such as a mouse or rat).’





”Relying on other models, such as colorectal, don’t apply, which makes this an unmet need. Epithelial neoplasms (new, abnormal tissue growth) of the appendix are rare, but without an effective way to study them, the opportunities to develop new treatments have also been rare,” said senior author Andrew Lowy, MD, chief of the Division of Surgical Oncology at Moores Cancer Center and a professor of surgery at UC San Diego School of Medicine. The obstacles to creating a preclinical model of appendiceal cancer are numerous:
- Access to clinical tissues is rare because the disease is rare.
- The majority of neoplasms have mucinous histology, a characteristic that makes them difficult to assess under a microscope and to culture.
- Mice do not have the equivalent of a human appendix, rendering them unsuitable as a model.
“We’ve learned that utilizing tissue slices made from patient tumor resections is great way to study the pathobiology of this disease, and we are hopeful they will help predict therapy responses in patients,” said Lowy. “Using this new model, we can now test new treatments that might lead to better outcomes for patients with advanced disease.”
Co-authors include: Jonathan Weitz, Tatiana Hurtado de Mendoza, Herve Tiriac, James Lee, Siming Sun, Bharti Garg, Jay Patel, Kevin Li, Joel Baumgartner, Kaitlin J. Kelly, Jula Veerapong, Morgan Hossein and Yuan Chen, all at UC San Diego.
Source-Eurekalert