Analysis of patient records using state-of-the-art data analytics can be done to predict future risk of metabolic syndrome, as demonstrated in research published in AJMC.
"The breakthrough in this study is that we are able to bring to light hyper-individualized patient predictions, including quantitatively identifying which individual patients are most at risk, which syndrome factors are most likely to push that patient past a threshold, and which interventions will have the greatest impact on that individual," said Colin Hill, co-founder and CEO of GNS. "The GNS automated data analytics platform paired with Aetna's deep clinical expertise produced these results on extremely large datasets in just three months, a testament to the ability of both groups."
GNS analyzed data from nearly 37,000 members of one of Aetna's employer customers who had voluntarily participated in screening for metabolic syndrome. The data analyzed included medical claims records, demographics, pharmacy claims, lab tests and biometric screening results over a two-year period. For this study, the Aetna and GNS teams utilized two distinct analytical models:
• A claims-based-only model to predict the probability of each of the five metabolic syndrome factors occurring for each study subject.
• A second model based on both claims and biometric data to predict whether each study subject is likely to get worse, improve or stay the same for each metabolic syndrome factor.
Both analytical models predicted future risk of metabolic syndrome on both a population and an individual level, with ROC/AUC (receiver operating characteristic/area under the curve) varying from 0.80 and 0.88. The researchers were able to develop detailed risk profiles for individual participants, enabling a deep understanding of exactly which combination of the five metabolic syndrome factors each of the study subjects exhibit and are at risk for developing. For every Aetna member whose data was used in the study, the researchers used a scale that measures the percentage risk that individuals have of exhibiting each of the five metabolic syndrome factors. For example, in an individual patient who exhibited two of the five risk factors, researchers could predict which third factor is the most likely to develop.
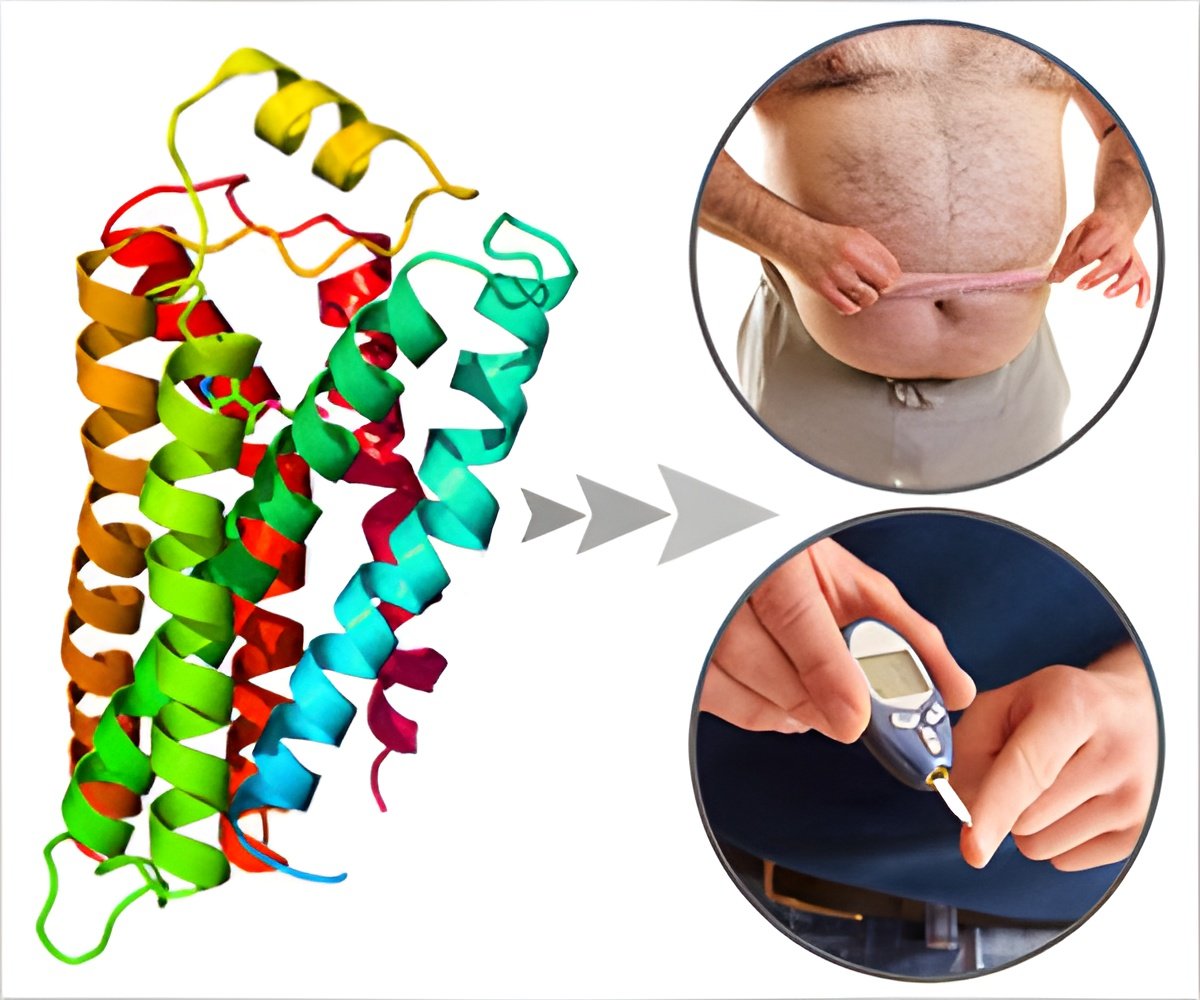
The analytical models also helped identify individual variable impact on risk associated with adherence to prescribed medications, as well as adherence to routine, scheduled outpatient doctor visits. A scheduled, outpatient visit with a primary care physician lowers the one-year probability of having metabolic syndrome in nearly 90 percent of individuals. In addition, the study found that improving waist circumference and blood glucose yielded the largest benefits on patients' subsequent risk and medical costs.
Advertisement














