Prioritizing patients for liver transplantation using the MELD-Na score, could increase the chances of high-risk patients receiving a transplant and reduce the risk of dying while on the waiting list.
‘Prioritizing patients for liver transplantation using the Model for End-stage Liver Disease Sodium (MELD-Na) score, instead of the more commonly used MELD score, could increase the chances of high-risk patients receiving a transplant and reduce the risk of dying while on the waiting list. ’





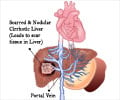
The MELD score, which estimates mortality risk for patients with end-stage liver disease using laboratory variables, has been used to prioritize patients on liver transplant lists for almost 20 years. Although MELD has been very successful in prioritizing patients, it does not accurately reflect the risk of death in patients with hyponatremia (low sodium levels), which is an important predictor of mortality in patients on liver transplant lists. The MELD-Na score, which includes serum sodium in the risk calculation, was adopted in the United States in 2016 for liver transplant prioritization, but is not yet used routinely across Europe. To test whether the use of the MELD-Na score in the Eurotransplant region (which includes Austria, Belgium, Croatia, Germany, Hungary, Luxembourg, the Netherlands, and Slovenia) could improve outcomes, the Leiden team evaluated 5,223 patients who were allocated onto the Eurotransplant liver transplant waiting list between 2007 and 2018 using their MELD scores. These patients were followed from their first listing to the time of delisting or until 90 days after listing. As part of the study, each patient was reclassified retrospectively based on their MELD-Na score, allowing an estimation of the number of lives saved if MELD-Na allocation had been used.
According to Dr Ben Goudsmit from Leiden University Medical Center, who presented the study results at this year's Digital International Liver Congress™, a large proportion (40%) of patients on the transplant waiting list had hyponatremia, and these patients had a three-fold increased risk of dying within 90 days of being listed.
'We also found that, if the MELD-Na score had been used to prioritize patients instead of the MELD score, 26.3% of those who died within 90 days would have had a significantly higher chance of receiving a liver transplant', he said. 'This equates to a 4.9% reduction in 90-day waiting-list mortality'.
The research team believes that, since there is a shortage of liver grafts and the prevalence of cirrhosis is increasing globally, better prediction of mortality and improved prioritization for liver transplantation are becoming increasingly important. 'We believe that MELD-Na-based allocation would help to prioritize patients on European liver transplant waiting lists and reduce the number of patients who die before they get the chance of receiving this life-saving treatment'.
Advertisement
Source-Eurekalert