Pregnant women appear to have worse clinical outcomes after thyroid and parathyroid surgery compared with their non-pregnant counterparts
A report in the May issue of Archives of Surgery, one of the JAMA/Archives journals, says that pregnant women appear to have worse clinical outcomes after thyroid and parathyroid surgery compared with their non-pregnant counterparts.
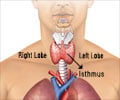
Thyroid and parathyroid surgery are used to treat cancer and other conditions. The incidence of thyroid cancer has increased by almost 250 percent over the last 30 years, increasing from 3.6 to 8.7 cases per 100,000 persons, according to background information in the article. The rate is almost double in pregnant women, with 14.4 cases per 100,000 persons. "Hyperthyroidism [overactive thyroid] has been reported in 0.1 percent to 0.4 percent of pregnancies. Inadequately treated hyperthyroidism during pregnancy poses significant risks to both mother and fetus," the authors write. "Outcomes after thyroid and parathyroid procedures during pregnancy have not been well characterized in the surgical literature."SreyRam Kuy, M.D., of Yale University School of Medicine, New Haven, Conn., and United States Department of Veterans Affairs, Washington, and colleagues compared clinical and economic outcomes of thyroid and parathyroid surgery performed on 201 pregnant women (average age 29) and a group of 31,155 age-matched, non-pregnant women from 1999 to 2005. Fetal, maternal and surgical complications as well as in-hospital death, length of stay and hospital costs were measured.
Of the 201 pregnant women, 165 underwent thyroid procedures and 36 underwent parathyroid procedures. "Compared with non-pregnant women, pregnant patients had a higher rate of endocrine [relating to glands that secrete hormones](15.9 percent vs. 8.1 percent) and general complications (11.4 percent vs. 3.6 percent), longer unadjusted lengths of stay (two days vs. one day) and higher unadjusted hospital costs ($6,873 vs. $5,963)," the authors write. "The fetal and maternal complication rates were 5.5 percent and 4.5 percent, respectively," Additionally, pregnant patients had higher surgical complications than non-pregnant patients for benign (27 percent vs. 14 percent) and malignant (21 percent vs. 8 percent) thyroid diseases while undergoing thyroidectomy (the surgical removal of part or all of the thyroid gland).
"Differences between pregnant and non-pregnant women in complication rates were most pronounced by diagnosis, race and hospital size," the authors note. When compared to non-pregnant women of the same race, white pregnant patients had double the complication rate (21 percent vs. 10 percent), black pregnant patients had nearly five times the complication rate (48 percent vs. 10 percent) and Hispanic pregnant patients had an almost three-fold higher complication rate (30 percent vs. 12 percent).
"These data suggest that thyroid and parathyroid surgery during pregnancy should be approached with caution and careful deliberation about whether the risks are outweighed by the benefits," the authors conclude. "Surgeon volume is an important predictor of outcomes, so pregnant women undergoing thyroid and parathyroid procedures should be directed to high-volume surgeons whenever possible. Disparities in outcomes based on race and insurance must be overcome. Optimizing maternal and fetal outcomes requires the collaboration of surgeons, endocrinologists, obstetricians, neonatologists, anesthesiologists, insurers and policy makers."
Source-Eurekalert
RAS