KTE-C19 produces complete remission, manageable toxicities in primary mediastinal B-cell lymphoma and transformed follicular lymphoma patients.

‘The KTE-C19, an autologous chimeric antigen receptor (CAR) T cell therapy, resulted in promising clinical activity in patients with refractory primary mediastinal B-cell lymphoma and transformed follicular lymphoma.’





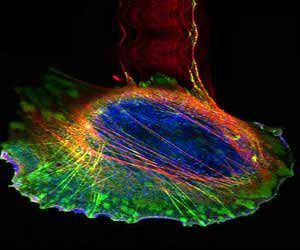
The ZUMA-1 study utilizes KTE-C19 which is an autologous chimeric
antigen receptor (CAR) T cell therapy. During KTE-C19 CAR-T therapy, T
cells are isolated from a patient's blood and genetically engineered in
Kite's laboratory to target the CD19 protein that is found on lymphoma
cells. The genetically engineered T cells are then infused within the
patient that they were originally harvested from. The KTE-C19 T cells
are able to recognize cancerous lymphoma cells that express CD19 and
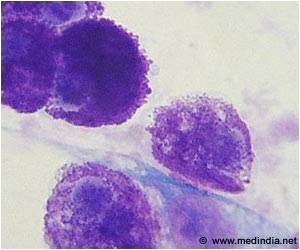
target them for destruction. The phase 1 portion of the ZUMA-1study revealed that KTE-C19 was tolerable and produced ongoing remissions in B-cell non-Hodgkin lymphoma patients (Locke et al, Abstr. 1048O, ESMO Congress 2016). The phase 2 portion of the study consists of two cohorts: cohort 1 for patients with chemo-refractory Diffuse Large B cell Lymphoma; and cohort 2 for patients with chemo-refractory primary mediastinal B-cell lymphoma or transformed follicular lymphoma.
As of June 16, six patients with refractory primary mediastinal B-cell lymphoma or transformed follicular lymphoma were treated in cohort 2 with KTE-C19. The patients were highly refractory to prior treatments and included three patients who were refractory to second-line or greater therapy and three patients who relapsed after autologous stem cell transplants.
KTE-C19 therapy resulted in promising clinical activity in these patients. With a median follow-up period of 3.2 months, all six patients achieved a complete remission. KTE-C19 treatment also resulted in manageable toxicities that were generally reversible. Grade 3 treatment-emergent adverse events occurred in 17% of patients and grade 4 treatment-emergent adverse events occurred in 67% of patients. All six patients experienced cytokine release syndrome; however, all cases were grade 1 or 2. Neurotoxicity occurred in 67% of patients and 33% of the cases were grade 3.
Source-Eurekalert