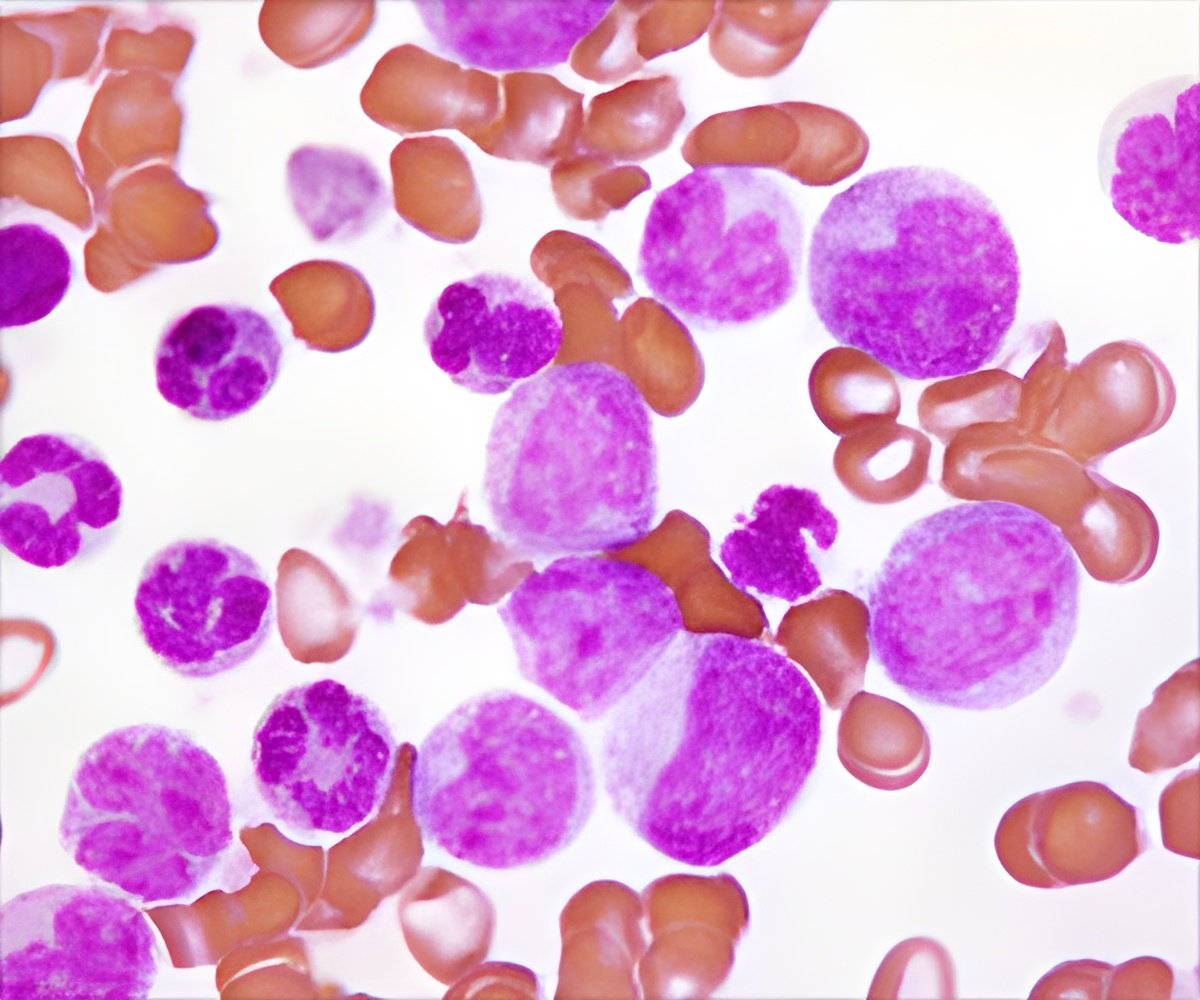
Chemotherapy and acute lymphoblastic leukemia impact patient’s immune systems, leaving them vulnerable to infections. Prophylactic antibiotics can reduce infection risk.
‘Administration of prophylactic antibiotics for children with acute lymphoblastic leukemia during the treatment phase reduces bacterial infection risk.’





The investigators, reporting their findings at the 57th annual meeting of the American Society of Hematology, found that prophylactic antibiotic treatment reduced the incidence of infection by approximately 60 percent compared to historic controls. Both ALL and the chemotherapy used to treat it impact patients' immune systems, leaving them vulnerable to infection by a variety of bacteria. The risk of infection is particularly high during the first or "induction" phase of ALL treatment, when oncologists attempt to push the leukemia into remission.
"Children who develop bacterial infections during induction can become severely ill and often need to be admitted to the intensive care unit," said study senior investigator Lewis B. Silverman, MD, clinical director of the Hematologic Malignancies Center at Dana-Farber/Boston Children's and principal investigator of the Dana-Farber Cancer Institute (DFCI) ALL Consortium clinical trials group.
"As a group, we realized that there was great variability among our institutions in terms of the management of leukemia patients who develop a fever. This study was designed to ask whether uniform guidelines for antibiotic prophylaxis and fever management could prevent infection-related morbidity and mortality in our patients. It was not clear, prior to starting the study, whether such a strategy would succeed, or whether the use of prophylaxis might increase the incidence of antibiotic-resistant infections or the frequency of fungal infections."
To determine whether preventive antibiotic treatment could reduce the rate of bacterial infections during induction therapy, the DFCI ALL Consortium added universal antibiotic prophylaxis to its 11-001 treatment protocol for pediatric ALL. Clinicians at nine sites participating in the consortium enrolled 229 newly diagnosed children with ALL on the protocol between 2012 and 2015.
Advertisement
The study's data indicate that the prophylactic strategy did indeed reduce infection risk. The proportion of patients given prophylactic antibiotics who experienced at least one infection during induction-phase therapy on protocol 11-001 was 13.1 percent, approximately 50 percent lower than the proportion among patients treated on protocol 05-001 (26.6 percent). The incidence of bacterial infection among children on protocol 11-001 was 9.9 percent, approximately 60 percent lower than that among children on protocol 05-001 (24.7 percent).
Advertisement
"While larger, randomized clinical trials are needed to confirm these findings, these are very exciting results," said Silverman. "The use of antibacterial prophylaxis appears to have made a profound difference for our patients."
Source-Eurekalert