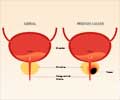
Two recently conducted large randomised trials suggest that prostate cancer screening has yet to prove its worth.
Two recently conducted large randomized trials suggest that prostate cancer screening has yet to prove its worth.
Published in CA: A Cancer Journal for Clinicians, a study report says that if there is a benefit of screening, it is, at best, small.Given that prostate cancer is virtually ubiquitous in men as they age, the report points out that it is clear that a goal of "finding more cancers" is not acceptable.
The authors instead say that public health principles demand that screening must reduce the risk of death from prostate cancer, reduce the suffering from prostate cancer, or reduce health care costs when compared with a non-screening scenario.
According to them, prostate cancer screening has yet to reach one of these standards to date.
The research team-including Dr. Otis W. Brawley of the American Cancer Society and Dr. Donna Ankerst and Dr. Ian M. Thompson of the University of Texas Health Science Center at San Antonio-agree that a decrease in prostate cancer death rates has been observed as compared to the mid-1980s, since when screening with the prostate-specific antigen (PSA) blood test has more than doubled the risk of a prostate cancer diagnosis.
They, however, say that the relative contribution of PSA testing as opposed to other factors, such as improved treatment, has been uncertain.
Advertisement
A similar model using data from Europe estimated a 50 percent overdiagnosis rate, they add.
Advertisement
The authors further say that over-diagnosis significantly affects 5-year survival statistics, making them uninformative in demonstrating progress in cancer control.
Their report says that the future of prostate cancer will include better screening tests, better methods to assess a man's risk of prostate cancer, and prevention strategies, including the use of finasteride, a drug currently used for the treatment of urinary symptoms related to prostate enlargement.
In another editorial, Dr. Peter Boyle of the International Prevention Research Institute, Lyon, France and report co-author Dr. Brawley say: "The real impact and tragedy of prostate cancer screening is the doubling of the lifetime risk of a diagnosis of prostate cancer with little if any decrease in the risk of dying from this disease."
The authors pointed out that in 1985, before PSA screening was available, an American man had an 8.7 percent lifetime risk of being diagnosed with prostate cancer and a 2.5 percent lifetime risk of dying from the disease.
Twenty years later, in 2005, an American man had a 17 percent lifetime risk of being diagnosed with prostate cancer and a 3 percent risk of dying from the disease.
According to the report, even in the best case scenario, applying the findings of a European trial that found PSA led to a 20 percent reduction in the risk of death, the average man who chooses screening decreases his risk of prostate cancer death from a lifetime risk of 3 percent to a lifetime risk of 2.4 percent.
In exchange, he doubles the chances of becoming a prostate cancer patient, his risk of diagnosis rising from about nine percent to at least 17 percent.
"Men should discuss the now quantifiable risks and benefits of having a PSA test with their physician, and then share in making an informed decision, and the weight of the decision should not be thrown into the patient's lap," the authors concluded.
Source-ANI
SRM






![Prostate Specific Antigen [PSA] Prostate Specific Antigen [PSA]](https://www.medindia.net/images/common/patientinfo/120_100/prostate-specific-antigen.jpg)