Questions are being raised about the safety of in-vitro fertilization. Both the mother and the baby could face several risks, it is felt.
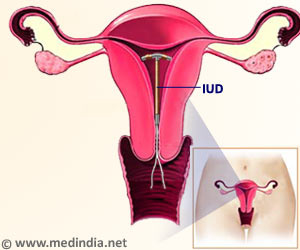
In vitro fertilization is becoming increasingly popular. More than three million babies worldwide are conceived through Assisted Reproductive Technologies (ART) — IVF, ovulation induction and intra-uterine induction.
In Britain, ART accounts for 1.4 per cent of all births every year — 10,242 in 2004 — while many more women undergo treatment unsuccessfully (the success rate among women under 35 is 28.2 per cent, falling to 10.6 per cent for those aged 40-42). But many have begun to wonder, like noted fertility expert Professor Robert Winston, “Can we really trust the science behind IVF?”Disturbing revelations are coming in from various studies. Researchers in the U.S. say that the common practice of storing fertilized embryos can provoke genetic changes that may develop into mental and behavioral disorders later in life. From Canada come claims that IVF can increase some birth defects tenfold; while from Denmark a study of young men finds those conceived through fertility treatment are 50 per cent more likely to be infertile themselves. Or is it just a 'mass experiment' with desperate women as the guinea pigs — and the results a time-bomb that future generations will have to defuse?
Louise Brown, the world’s first test tube baby, was born in 1978 and became a mother herself last year. Her son, Cameron, was conceived naturally and this was hailed in some quarters as proof that IVF really 'works'. Others, however, caution against attributing too much significance to this happy event. The treatment that led to Louise’s birth, they point out, was very different from today's.
Doctors waited until one of her mother Lesley's eggs had ripened, collected it and then fertilized it in a test tube with her husband's sperm before replacing it in her womb. Since then, procedures have moved become more and more complex. The main developments in ART have focused on manipulating the production of a woman's eggs through the administration of fertility drugs. This has been both to control the timing of ovulation and to increase the number of eggs produced. The more eggs, the logic goes, the higher the chance of a successful pregnancy.
Once harvested, the eggs are fertilised in the lab while the woman receives hormone drugs to ready her womb for implantation. It is then hoped a normal pregnancy will ensue. But see what happened to Lee Cowden, aching to conceive and who was pumped full of hormones to make her produce more eggs. The result? A trip to hospital — but not to a maternity suite.
"I was 25 and felt this excruciating pain in my chest," recalls Lee, a music therapist from Surrey. "I was rushed into intensive care in an ambulance, and it became pretty clear that, despite my age, I had suffered a heart attack. "I'd suffered a clot caused by the fertility treatment I had undergone. I remember lying in my hospital bed, desperately worried. Not for my health, but because I thought that they’d never let me have IVF again, and I'd never become a mother." With relatively small provision of IVF on the NHS, the fertility business has developed into a multi-million-pound industry charging up to £5,000 for a single cycle.
Advertisement
But the Human Fertilisation And Embryology Authority (HFEA), which licenses fertility clinics, is running a public consultation to examine whether single-embryo implantation should become the norm. While this shift will address the problems associated with multiple births, it's not the end of the matter. For reasons that remain unclear, there are also higher incidences of post-birth difficulties with single IVF babies.
This question of second-generation infertility is an area of particular interest, and given the relative infancy of the science of IVF, it is something that will become clear only in years to come. At the same time it is also acknowledged that the risks remain small - in other words, if a natural child has a one-in-5,000 risk of a deformity, even if the risk doubles through IVF it remains a remote possibility. But medics insist it cannot be entirely ignored.
"The risks certainly aren't so big that we should not use this technology, but we should use it cautiously," says Professor William Ledger, professor of obstetrics and gynaecology at the University of Sheffield. Possibly more and more people are turning to IVF almost as a lifestyle choice, as a convenience, and that could have damaging consequences in the long run. There is a fairy tale ending to the story of the 28-year-old Lee Cowden. Following her heart attack in 2004, Lee — who was infertile after being diagnosed with polycystic ovary syndrome as a teenager — was told it was too dangerous for her to continue with conventional IVF.
But another tried a low-dose treatment on her and within three months of starting treatment she became pregnant. "I cried my eyes out when the nurse finally said: "Your pregnancy test is positive." I was so happy." Lee's daughter Molly was born last November and is doing well.
"Following the heart attack, I kept thinking it was only a matter of time before doctors told me I'd never be able to have children. "I've been on a roller-coaster ride, with some agonising times…:” Not all could be similarly lucky, it is pointed out.
Source-Medindia
GPL/S