the use of a short one week course of radiation before surgery for rectal cancer leads to a reduced risk of recurrence
An international study presented September 22, 2008, at the American Society for Therapeutic Radiology and Oncology’s 50th Annual Meeting in Boston has indicated that the use of a short one week course of radiation before surgery for rectal cancer leads to a reduced risk of recurrence but with some impairment in quality of life for sexual and bowel function.
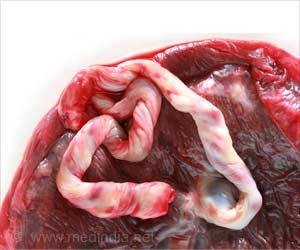
The primary treatment for rectal cancer is surgery. Traditionally, cancer found in the lower 15 centimeters of the bowel (rectum) is surgically removed. However, simply removing the tumor leaves a risk of cancer re-growth within the bowel and surrounding tissues. Not only is this recurrence incurable in the majority of patients, but it can cause side effects that are difficult to control. Depending on the location and stage of the cancer, doctors may also recommend radiation therapy and chemotherapy, which can be given before or after surgery.The Medical Research Council CR07 trial looked at data from 1,350 patients throughout the United Kingdom, Canada, South Africa and New Zealand. The trial compared routine use of a one week course of radiotherapy before surgery (pre-operative) with a selective use of radiotherapy after surgery (post-operative) to reduce the risk of recurrence. In the post-operative group, patients at high risk of a local recurrence received 25 treatments of radiotherapy daily over a five-week period combined with chemotherapy after surgery.
Comparison of the overall treatment approaches found that only 4 percent of patients in the pre-operative group had local recurrence of the cancer after three years, compared with 11 percent of patients the post-op group. It also found that pre-operative patients had a higher chance (78 percent) of being alive without cancer recurrence five years later than the post-op patients (72 percent).
To assess the impact of the treatments on quality of life, patients completed two detailed questionaires prior to treatment and on a regular basis for three years. The results show that physical functioning was decreased at three months, but then returned to previous levels, indicating that patients appear to recover well from their treatment in most cases.
The quality-of-life study showed that male sexual function deteriorated at three months and this appeared to be due to surgery. There was a further smaller deterioration thereafter due to the use of pre-operative radiotherapy. There was also a difference in bowel function due to the pre-operative radiotherapy.
“We know that this and other trials have consistently shown that radiation before surgery reduces the risk of local cancer returning, however, this has to be balanced against any negative side effects,” David Sebag-Montefiore, M.D., principal investigator of the study and a radiation oncologist at the St. James' Insitute of Oncology in Leeds, United Kingdom, said. “The results of our quality of life study should help doctors and patients to discuss both the benefits and risks of pre-operative radiation before surgical removal of rectal cancer.”
Advertisement
RAS/SK