Rapamycin, an FDA-approved drug already on the market, has the potential to become the first effective treatment to prevent heterotopic ossification.
‘Since rapamycin is an FDA-approved drug, this makes it a promising candidate for fast-track translation in the clinic.
’





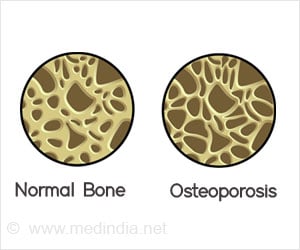
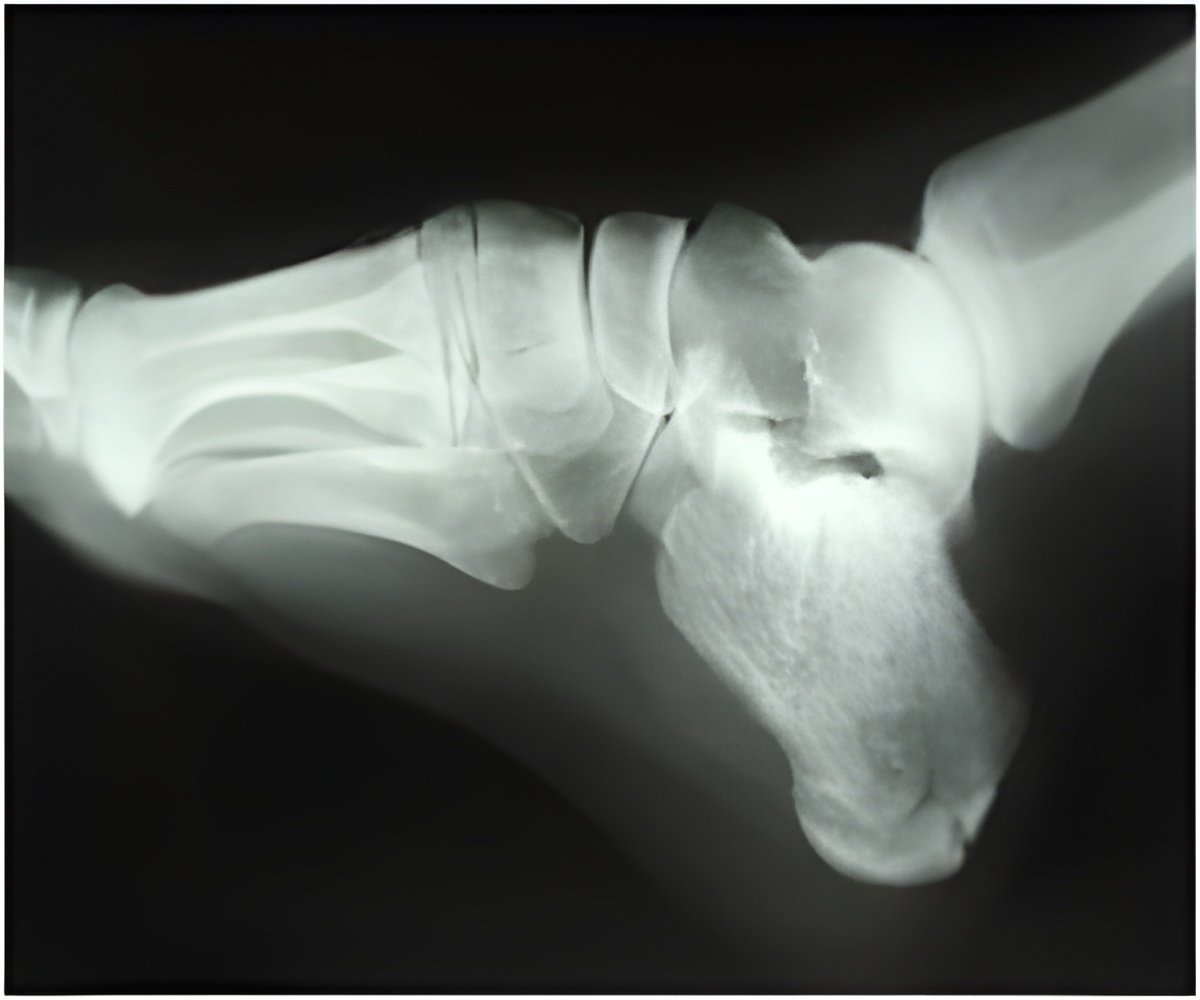
"HO is a significant complication of combat-related blast trauma and is described by clinicians as the single most critical barrier to functional mobility, independence, and return to military service. Despite the exceptionally high rate of HO in combat-injured military personnel (estimated at about 65%), there still remains no primary prophylactic regimen. The standard of care is surgical resection, but even with surgical resection, most patients fail to regain their normal range of motion and often suffer from chronic pain and joint contractures," explained Thomas A. Davis, PhD, Vice Deputy Chair of Research, Department of Surgery, Uniformed Services University, the Walter Reed National Military Medical Center (Bethesda, MD), and the Naval Medical Research Center (Silver Spring, MD). The study used a proven rodent model of HO that mimics the injuries seen in combat casualties. The model replicates blast-related limb injury, femoral fracture, quadriceps crush injury amputation, and infection with methicillin-resistant Staphylococcus aureus (MRSA). Using the model, the researchers demonstrated a significant reduction of HO in animals treated with rapamycin. For instance, 2.5 mg/kg of rapamycin for 14 days resulted in a 90% reduction of total new bone and 83% reduction in soft tissue ectopic bone compared to controls at 84 days after injury.
Additionally, the treatment reduced the number of progenitor cells in injured tissue that give rise to abnormal bone formation. It also decreased the gene expression of key factors associated with extracellular matrix remodelling, bone formation, inflammation, and blood vessel formation.
These findings are important because they define a potential prophylactic strategy to prevent HO in combat casualties and civilians at high risk of this disabling condition, thereby dramatically improving the function and quality of life of patients at risk. They indicate that mammalian target of rapamycin (Mtor)-dependent inhibition is a viable therapeutic option to prevent the development of blast trauma-induced HO. "Given the fact that rapamycin is an FDA-approved drug makes it a promising candidate for fast-track translation in the clinic. We are cautiously optimistic, appreciating that the transition from laboratory animal models to the clinical setting is often challenging," commented Dr. Davis.
Rapamycin (Sirolimus) is a bacterial macrolide that is FDA-approved for use as an immunosuppressant, such as preventing rejection of kidney transplants. Through the mTOR signalling pathway, it is involved in the regulation of many cellular processes, including cell survival, metabolism, proliferation, differentiation, and senescence. In the model used in this study, although rapamycin had an anti-angiogenic effect (as indicated for example by less blood vessel formation in the injured site), it did not delay wound closure or affect wound healing.
Advertisement