The knowledge base to tie together all the diverse symptoms which are now known as part of endometriosis has been updated.
Symptoms can include pain in the pelvis, abdomen, thighs, back, and bladder, along with period pain, pain during or after sex, infertility, fatigue, bowel symptoms, headaches, nausea, depression and anxiety.
‘Using ultrasound scan imaging of the pelvis for endometriosis diagnosis has advantages over laparoscopy, including reduced cost and reduced risk of complications.’





Advertisement
Why it is Important to Understand the Pathophysiology?
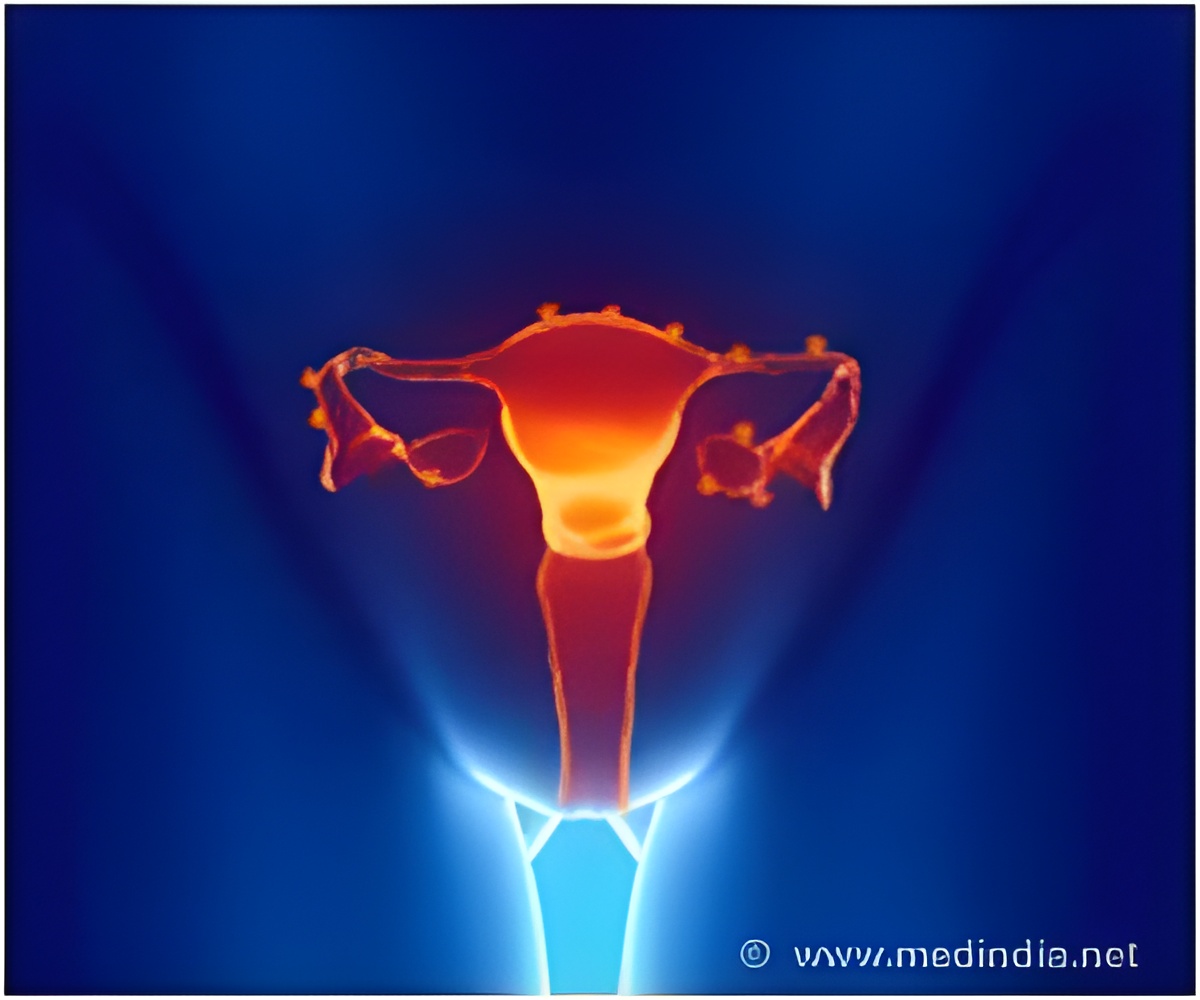
Endometriosis is characterized by endometrium-like tissue existing outside of the uterus, usually involving the pelvic organs. Essentially, every month you get a pain trigger when all the dead endometriosis cells break down in response to the hormones and it causes an inflammatory response.The inflammatory response triggers a nerve in the back, which causes back pain and then it sensitizes all the organs, so people get irritable bowel symptoms, bladder pain, pain with intercourse and they also get stabbing pain, which is a muscle spasm of the pelvic floor.
Patients can also get central sensitization, which is headaches or fatigue and sometimes vomiting or nausea and feeling hot and cold.
Advertisement
Asking the Right Questions for Endometriosis
The average delay between onset of endometriosis symptoms and diagnosis is 7–12 years. There are also many differential diagnoses, including inflammatory bowel disease, urinary tract infections, and pelvic inflammatory disease.Efficiently diagnosing endometriosis meant asking patients not only about period pain but also about the other symptoms described above. Doctors should work through the questions about the impact of period pain and other symptoms on daily life to create an endometriosis risk score.
If a woman comes to a general physician with concerns about their menstrual cycle or fertility they should be referred to either a gynecologist, sooner rather than later.
There’s good evidence to suggest that by the time someone comes wanting fertility treatment, if the endometriosis diagnosis has been delayed, then their outcomes are far worse than if they were diagnosed and treated earlier.
Advertisement
Getting The Right Scan For Endometriosis
Laparoscopy is recognized in guidelines around the world as the diagnostic gold standard for endometriosis, including by the Royal Australian New Zealand College of Obstetricians and Gynaecologists.However, the European Fertility Society said this should no longer be the case and that endometriosis findings on a scan could be considered diagnostic. Laparoscopy is recommended only in patients with negative imaging results, or where empirical treatment was unsuccessful or inappropriate.
Firstly, even with a negative scan, there’s still a 30% chance the patient has endometriosis. Secondly, only a specialized transvaginal ultrasound or MRI (magnetic resonance imaging) will do.
Putting Surgery in its Right Place
Laparoscopic surgery to remove endometriosis lesions could alleviate some of the pain associated with endometriosis as well as improve fertility.Most experienced surgeons would offer diagnosis and excision in the same operation. Ideally, the patient should require only a single laparoscopy for disease excision and subsequently have their diseases managed by endometrial suppressive therapy, such as an intrauterine device or the pill, she added.
A minority of women who underwent specialist endometrial surgery had significant recurring symptoms after surgery, she said. In those cases, doctors would usually suggest a few years of symptom management with suppressive therapy before considering surgery again.
For women with chronic pelvic pain where muscle spasms or central sensitization have occurred, surgery has less of a role, and management with a multidisciplinary team including physiotherapy and pain specialists becomes more important.
This stressed the importance of setting up a chronic disease care plan for endometriosis patients and doctors should be aware of this.
Source-Medindia












