Increasing general practice opening hours would improve the opportunity for assessment and urgent referral to specialist care of patients with a transient ischaemic attack (TIA) or minor stroke
Increasing general practice opening hours would improve the opportunity for assessment and urgent referral to specialist care of patients with a transient ischaemic attack (TIA) or minor stroke, which could prevent over 500 recurrent strokes a year in England alone, concludes a study published on bmj.com today.
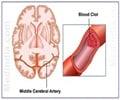
Recent research shows that early assessment and treatment after a TIA and minor stroke can significantly reduce the risk of recurrent disabling or fatal stroke. The national stroke strategy and guidance from the National Institute of Health and Clinical Excellence (NICE) recommend that high risk patients must be seen within 24 hours of symptom onset.In the UK, most patients choose to seek help from their general practice after TIA or minor stroke rather than via the emergency services.
Recent proposals to change the GP contract and increase general practices' opening hours from office hours (8am–630pm Monday to Friday) to include evenings and weekends, could improve access to primary care and may influence patients’ healthcare seeking behaviour and affect clinical outcomes, particularly in emergency cases such as patients with TIA and minor stroke.
Dr Daniel Lasserson and colleagues from the University of Oxford assessed the potential impact on stroke prevention of increasing primary care opening hours to 8am–8pm daily. They analysed the healthcare seeking behaviour of 91,000 patients registered at nine general practices in Oxfordshire between 1 April 2002 and 31 March 2006.
The researchers recorded the time of symptom onset, time to calling healthcare services, and the choice of healthcare provider in patients with a definite or probable TIA or minor stroke.
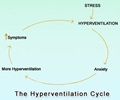
They found that current opening hours can increase the delay in assessment. Most patients who had a TIA or minor stroke out of hours delayed seeking health care until their registered general practice was open, causing long delays in seeking treatment, particularly at weekends.
Advertisement
Thirteen patients who presented with a stroke had a previous TIA or minor stroke out of hours and did not seek emergency care.
Advertisement
The authors conclude by calling for studies to examine the reasons for patients’ choice of healthcare provider after TIA and minor stroke, and the reasons for the delay in seeking health care which could help inform effective public health awareness campaigns.
In an accompanying editorial, Moyez Jiwa from the Curtin Health Innovation Research Institute in Perth and Andrew Knight from the University of Sydney, say that the findings confirm that delay in access to health services has serious consequences and should be a target for improvement.
However, they suggest that public health messages alerting patients with symptoms of TIA to the need for emergency care would be of more benefit than extending general practice opening hours.
Source-BMJ
LIN