Methods to improve understanding about obesity and cancer are being developed by researchers at the National Institute for Aging.
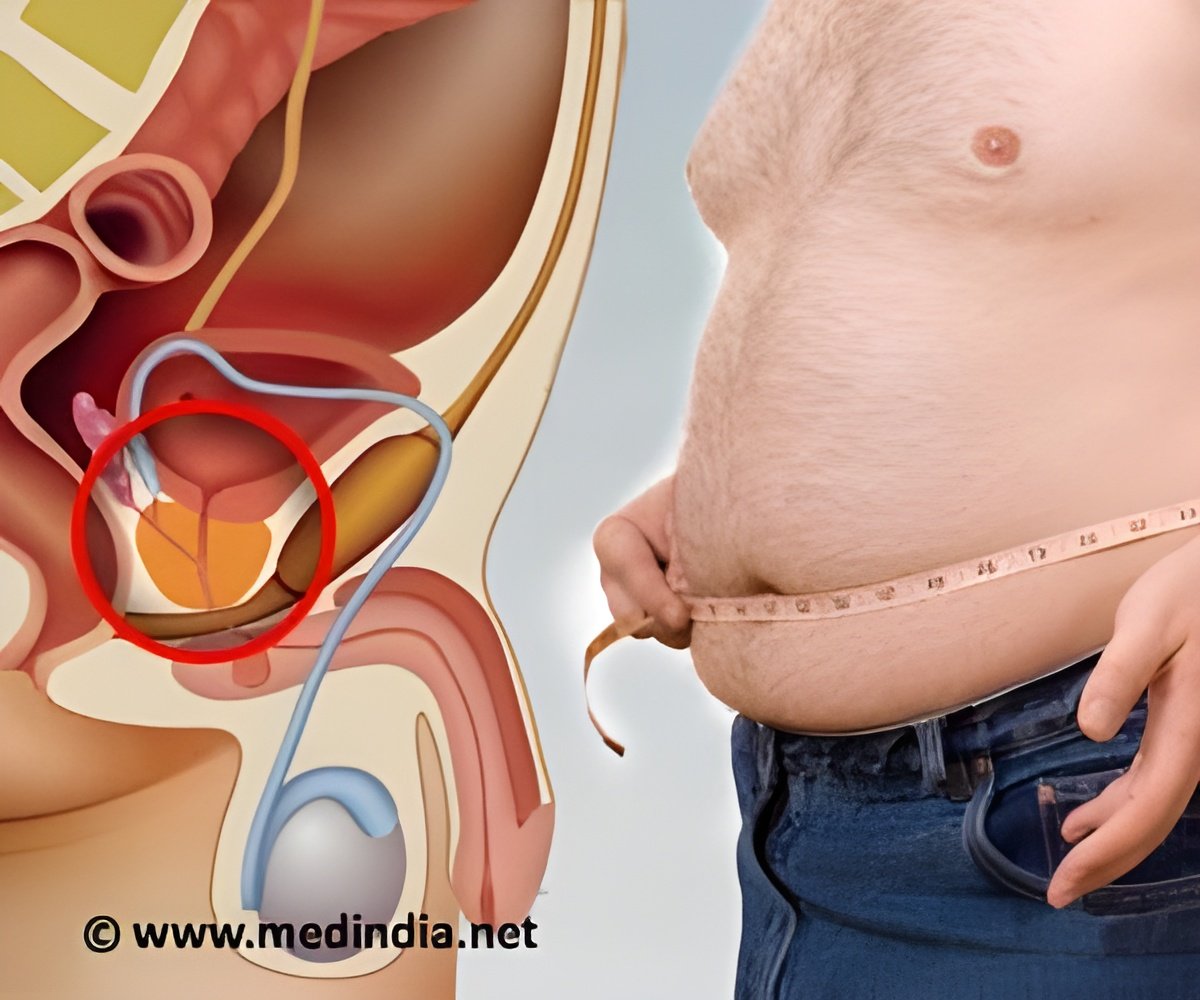
According to the study, "results suggest that adiposity may carry risk for cancers beyond those identified as obesity-related by the National Cancer Institute and further suggest a possible sex differential with respect to adipose and cancer risk."
Dr. Rachel Murphy, lead author on the study, is a researcher at the Laboratory of Epidemiology, and Population Sciences, Intramural Research Program, National Institute on Aging, in Bethesda, Maryland.
She said, "I think it's important to realize that BMI is not the only indicator of health to concentrate on. After controlling for risk factors we found that greater fat confers risk for cancer in older men and women. For example, women with more overall fat mass and more visceral fat had a higher risk of developing cancer."
"For men, greater visceral adipose was a particularly strong risk factor for many types of cancer regardless of the individual's BMI. Men with the most visceral fat had a nearly 3 times higher risk of many types of cancer (esophagus, pancreas, colon and rectum, kidney, thyroid, and gallbladder) compared to men with little visceral fat. When we controlled for BMI, the risk for visceral fat was strengthened."
"These findings provide new insight into obesity and cancer in old age, and suggest that interventions to target visceral adipose in addition to promotion of healthy body weight may impact future cancer risk."
Advertisement