When perioperative continuous insulin infusion protocols are implemented, achieving Surgical Care Improvement Project (SCIP) benchmarks for glycemic control may be irrelevant
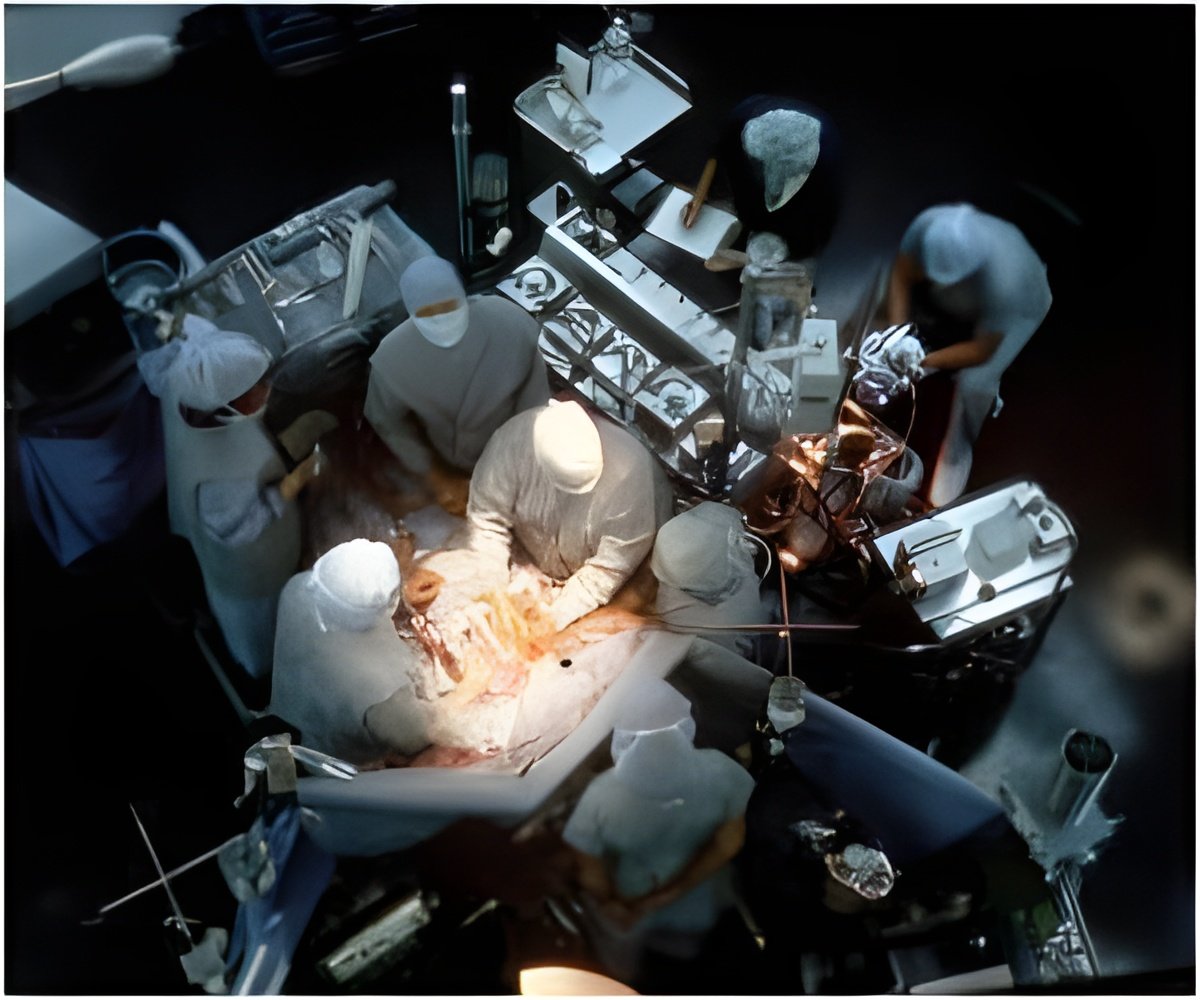
Currently, 40 percent of all patients undergoing CABG suffer from diabetes, and this number is quickly rising. Traditionally these patients have more complications following surgery, including greater risk of heart attacks, more wound infections and reduced long-term survival. Previous studies from BMC have shown that patients receiving insulin infusions during surgery and in the postoperative period to achieve blood glucose levels of less than 200mg/dl have significantly less morbidity and mortality. As a result of these pioneering studies, national guidelines now mandate that all CABG patients receive an intravenous insulin infusion when necessary to maintain blood glucose levels of less than 200mg/dl in the perioperative period.
SCIP has benchmarked 6 a.m. blood glucose of less than 200 mg/dl on post-operative day one and day two as a quality measure of glycemic control in cardiac surgery to be used for reporting of operative outcomes and monetary reimbursement. However, the relevance of SCIP in patients already receiving continuous insulin infusions, designed to achieve optimal glycemic control, is unknown. Hospitals in which SCIP outliers are present may be publicly cited for poor glycemic control and receive less monetary reimbursement. It is important, therefore, to determine whether SCIP is a valid marker of glycemic control in CABG patients.
Between January 2006 and April 2011, 833 patients underwent CABG surgery at BMC and received continuous insulin infusions to maintain serum blood glucose of less than 180 mg/dl. Patients were divided into two groups: patients compliant with SCIP and those who were outliers-those who fell outside of the SCIP guidelines.
The researchers found the incidence of SCIP outliers to be 6.6 percent. These patients were more likely to suffer from insulin-dependent diabetes, have a higher hemoglobin A1c level which is indicative of poor glucose control in the months preceeding surgery, higher body mass and lower ejection fraction. "However, patients who were SCIP outliers had no increase in morbidity, mortality or hospital length of stay," explained senior author Harold Lazar, MD, a cardiothoracic surgeon at BMC and professor of cardiothoracic surgery at Boston University School of Medicine.
According to Lazar these findings may have national implications and may result in changes in guidelines for glycemic control. "We found that these patients may have had excellent glycemic control except for that one 6AM glucose level," added Lazar. A better index of glycemic control is to look at the percentage of time that a patients' glucose was less than 200mg/dl over 48 hours and not just one or two arbitrary points in time. "On the other hand, we saw patients who had poor glycemic control but just happened to have a glucose level of less than 200mg/dl at the two time periods measured by SCIP."
Advertisement
Advertisement