The way in which the functionality of genetically engineered T cells administered therapeutically to patients with melanoma changed over time has been characterized.

Early clinical research has indicated that cell-based immunotherapies for cancer, in particular melanoma, have potential because patients treated with antitumor T cells frequently have an initial tumor response; however, those responses are often transient.
"The cell-based immunotherapy we utilized was that of genetically engineered T cells," said James R. Heath, Ph.D., Elizabeth W. Gilloon Professor of Chemistry at the California Institute of Technology in Pasadena, Calif. "This approach is the most widely applicable way to generate large numbers of highly functional antitumor T cells."
Different T cell functions are associated with distinct proteins. Heath and colleagues took a closer look at how genetically engineered T cells functioned or failed after being transferred into patients. To do this, they used a recently developed, multiplexed technology that gave them a high-resolution view of which function-associated proteins individual cells expressed.
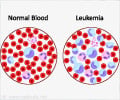
The researchers analyzed T cells isolated from blood samples taken from three patients with melanoma at several time points after treatment with genetically engineered antimelanoma T cells. Each of the patients from whom samples were taken had exhibited a different level of response to the immunotherapy.
The most highly functioning genetically engineered antimelanoma T cells made up about 10 percent of the total population of transferred T cells.
Advertisement
Although these highly functioning genetically engineered T cells had high tumor-killing capabilities when a patient first received them, those capabilities disappeared within two to three weeks.
Advertisement
These new T cells appeared to be a byproduct, through a process known as epitope spreading, of the original genetically engineered, tumor-killing T cells the patient received, Heath explained. The researchers also discovered one potential cause for the transient response to T cell therapy. Results showed that as the patient's own immune system recovered, after its initial depletion prior to therapy, those recovering T cells appeared to inhibit the antitumor immune response.
Source-Eurekalert