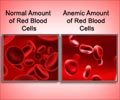
The restrictive strategy of blood transfusion in heart attack patients with anemia is 84% cost-effective compared to the liberal approach, in addition to improving cardiac clinical outcome of patients, with less chance of developing an infection or acute lung injury.

‘Use of the restrictive strategy for blood transfusion in heart attack patients with anemia is safe, saves blood, and effectively prevents 30-day cardiac events.’
Read More..




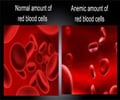
However, there is uncertainty over the benefits of blood transfusion in these patients. Observational studies have reported that transfusion is associated with a higher rate of mortality in patients with myocardial infarction. The optimal transfusion strategy in patients with acute myocardial infarction and anemia is also unclear. Only two very small randomized trials have been conducted, with conflicting results. Read More..
REALITY is the largest randomized trial comparing a restrictive versus a liberal blood transfusion strategy in myocardial infarction patients with anemia. In the restrictive strategy, transfusion was withheld unless haemoglobin dropped to 8 g/dL. In the liberal strategy, transfusion was given as soon as haemoglobin was 10 g/dL or below. Previous trials have compared these two strategies in other settings such as gastrointestinal bleeding, cardiac surgery, or non-cardiac surgery, but patients with acute myocardial infarction were excluded.
There were two primary endpoints. The primary clinical endpoint was a composite of major adverse cardiac events (MACE) at 30 days, including all-cause death, myocardial infarction, stroke, and emergency percutaneous coronary intervention (PCI) prompted by myocardial ischemia. The cost-effectiveness endpoint was the incremental cost-effectiveness ratio (ICER) at 30 days.
Principal investigator Professor Philippe Gabriel Steg of Hospital Bichat, Paris, France explained the reasons for having both a clinical and cost-effectiveness outcome: "Our hypothesis was that in myocardial infarction patients with anemia, a restrictive strategy would be non-inferior to a liberal strategy with respect to clinical outcomes at 30 days but would be less costly."
The trial was conducted in 35 hospitals in France and Spain. It enrolled 668 patients with acute myocardial infarction and anemia (haemoglobin 10 g/dL or below, but above 7 g/dL) at any time during admission. Patients were randomly allocated to the restrictive or liberal transfusion strategy and followed-up for 30 days.
Advertisement
Cost-effectiveness analysis indicated that the restrictive strategy had an 84% probability of being cost-saving while improving clinical outcomes, i.e. "dominant" from a medico-economic standpoint.
Advertisement
Professor Steg said: "Blood is a precious resource, and transfusion is costly, logistically cumbersome, and has side effects. The REALITY trial supports the use of a restrictive strategy for blood transfusion in myocardial infarction patients with anemia. The restrictive strategy saves blood, is safe, and is at least as effective in preventing 30-day cardiac events compared to a liberal strategy while saving money."
Source-Eurekalert