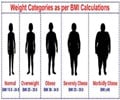
Body Mass Index (BMI) might not be a best obesity indicator to assess risk for lung cancer.

‘Body Mass Index (BMI) might not be the best obesity indicator to assess risk for lung cancer. This might be probably because the body mass index fails to discriminate between fat and lean body mass and also account for body fat distribution. Hence CT scans may provide a measurement of excess body weight using visceral fat index and predict the better outcomes of lung cancer.’





It is increasingly recognized that 'visceral' or 'central obesity' is the primary driver to high body fat and its outcomes. Although the BMI is easy to measure, its critics lie in its inability to discriminate between fat and lean body mass and also account for body fat distribution. "Based on the established knowledge described above, we sought to measure central obesity in a cohort of [patients with] stage I NSCLC [who were] undergoing lobectomy at our institution and examine its association with oncologic outcomes," says Joseph Barbi, Ph.D., first author of the manuscript.
The study team thereby examined 554 patients with stage I and II NSCLC – lung cancer before they underwent lobectomy surgery and calculated their excess body weight using visceral fat index measured by CT scans.
Because patients with early-stage disease are typically treated with surgery alone, without other treatments that may complicate the analysis, the researchers believed they provide a context where the relationship between central obesity and tumor progression can be studied without additional therapy-associated confounders.
Visceral Fat and Lung Cancer Outcomes
Advertisement
Interobserver correlation of VFI measurements was good. The correlation of measurements between L2 and L3 and between L1 and L3 levels was also good. Therefore, in the few cases where measurements at L3 were not available, measurements at L2 or L1 were used.
Advertisement
The team also report that an apparently multifaceted immune dysfunction prevalent in the tumors of obese mice and patients might suggest a common potential mechanism for the accelerating effect of obesity on the development of tumor burden in the obese.
"Our study provides much needed clarity to the relationship between adiposity and NSCLC patient survival, providing firm scientific justification for the targeting of obesity's pro-tumor effects, which include decidedly adverse effects on the antitumor immune response. Our findings also reaffirm the utility and relevance of available mouse models to study further the mechanisms of obesity's lung cancer-promoting effects. Importantly, they also validate a refined approach for studying obesity in retrospective data sets [of patients with cancer]," says Dr. Sai Yendamuri, M.D., from Rosewell Comprehensive Cancer Cancer in Buffalo, N.Y., who led the study.
The study thereby highlights the fact that visceral obesity is associated with overall poor and recurrence-free survival in patients with early NSCLC. Hence the continued efforts to better predict lung cancer outcomes aids in the development of novel therapeutic approaches to prevent or control early-stage lung cancers
Source-Medindia