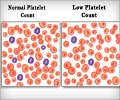
Increased risk or bleeding associated with low platelet counts was noted in patients who had undergone hemodialysis using dialyzers that had been sterilized with the use of electron beams.
Mercedeh Kiaii, M.D., F.R.C.P.C., of the University of British Columbia, Vancouver, Canada, and colleagues conducted a study to determine the prevalence and cause of thrombocytopenia in patients undergoing hemodialysis in British Columbia and southern Alberta province between April 2009 and November 2010. Retrospective analyses of historical patient, laboratory, and dialyzer data predating conversion to e-beam dialyzers were undertaken, with prospective collection of predialysis and postdialysis platelet counts before and after the change from e-beam to non-e-beam sterilized dialyzers in September 2009. Significant thrombocytopenia was defined as post-dialysis treatment platelet count of less than 100 x 103/µL and a postdialysis decrease in platelet count of more than 15 percent.
Province-wide testing of all patients from British Columbia who underwent hemodialysis in community and hospital-based facilities permitted collection of data from the majority (80 percent) of patients with hemodialysis from British Columbia (1,706 of 2,146 patients) and from Alberta (425 patients). Of the 1,706 patients from British Columbia, 1,411 patients (83 percent) were undergoing dialysis using e-beam sterilized membranes. In British Columbia, 11.4 percent of patients (n = 194) had postdialysis platelet counts of less than 100 x 103/µL, 23.4 percent of patients (n = 400) had more than 15 percent decrease in platelet count postdialysis, and 7.2 percent of patients (n= 123) met both criteria. Similar proportions from the Alberta population who were undergoing dialysis using a polysulfone e-beam sterilized dialyzer made by a different manufacturer were demonstrated (10.8 percent; n=46 had postdialysis platelet counts of less than 100 x 103/µL; 32.0 percent; n= 156 had more than 15 percent decrease in platelet count postdialysis; and 7.3 percent (n = 31) met both criteria.
In multivariate analysis adjusting for patient and dialysis history characteristics, use of an e-beam sterilized dialyzer was associated with a 2.5 times increased risk of significant thrombocytopenia. "Overall, among 1,784 patients, there were significant reductions in postdialysis thrombocytopenia following the change to use of non-e-beam sterilized dialyzers, such that 120 patients (6.7 percent) had platelet counts of less than 100 x 103/µL; 167 patients (9.4 percent) had decreases in platelet counts of greater than 15 percent; and 38 patients (2.1 percent) met both criteria," the authors write.
"Our study highlights 2 important points in the care of patients undergoing hemodialysis. First, dialyzer reactions such as thrombocytopenia can occur even with the use of current technologically advanced dialyzer membranes and devices. Second, these reactions may be overlooked with current routine predialysis blood work. Hemodialysis unit protocols and guidelines might consider adding postdialysis blood counts to routinely performed blood work when new dialyzers are introduced to help identify possible dialyzer-associated adverse effects," the authors write.
The researchers add that it is biologically plausible that e-beam sterilization could induce changes in platelets by a number of possible mechanisms, but none of these have been thoroughly evaluated.
Advertisement
Editor's Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Advertisement
In an accompanying editorial, Jonathan Himmelfarb, M.D., of the University of Washington, Seattle, comments on the findings of this study.
"This systematic, multifaceted study clearly demonstrated a robust association of thrombocytopenia risk with use of e-beam sterilization of dialyzers. It is also an exemplary model for investigating other problems that can affect patient safety during complex procedures such as dialysis. Several recently published single-patient case reports also have implicated e-beam sterilization as a possible cause of dialysis-induced thrombocytopenia."
Source-Eurekalert