Patients with Atrial fibrillation when admitted into rural hospitals may have seventeen percentage higher risk of death during hospitalization

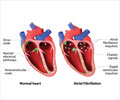
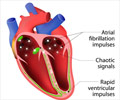
‘AF is a common problem, consisting of skipped or irregular heartbeats (arrhythmias) that can lead to blood clots, stroke, heart failure, and other cardiovascular complications. Left untreated, AF can double the risk of heart-related deaths’





"The identification of healthcare disparities is of utmost importance at this time to improve the overall care that is delivered in our healthcare system," explained lead investigator Wesley T. O’Neal, MD, MPH, of the Department of Medicine, Division of Cardiology, Emory University School of Medicine, Atlanta, GA. "Our research shows that urban-rural differences exist regarding the risk of hospital mortality among patients who are admitted for AF."Investigators used data from the National Inpatient Sample (NIS), a database representative of discharged patients from U.S. community hospitals, to compare the in-hospital mortality of patients admitted for AF in rural versus urban hospitals. The NIS approximates a 20% stratified sample of all discharges and excludes rehabilitation and long-term acute care hospitals.
The data are drawn from 44 states, plus the District of Columbia, representing more than 96 percent of the United States population. The analysis employed a cross-sectional examination of the NIS database of AF hospitalizations between 2012 and 2014 to determine if admission to a rural hospital was associated with an increased risk of in-hospital mortality compared with patients admitted to urban hospitals.
Looking at death due to any cause during hospitalization of patients with AF, the study found that patients admitted to rural hospitals had a 17% increased risk of death during hospitalization compared with urban hospitals. Analysis accounted for differences in patient characteristics and potential confounders. The five most common secondary diagnoses for patients hospitalized for AF were heart failure, hypertension, hyperlipidemia, diabetes, and acute kidney injury.
"Since we have identified rural hospitals as locations where in-hospital mortality for atrial fibrillation admission is possibly higher than other areas of the country, our findings will drive future research endeavors to uncover the reasons for this difference, and to develop strategies to improve the medical care for patients with this heart rhythm disturbance," Dr. O’Neal concluded.
Advertisement
In an accompanying editorial, Thomas F. Deering, MD, FHRS, and Ashish A. Bhimani, MD, FHRS, both from the Arrhythmia Center, Piedmont Heart Institute, Atlanta, GA, commend O’Neal et al for their detailed analysis, increasing awareness in the medical community about a potentially important arrhythmic healthcare issue, and placing their findings into the appropriate context. They also point out that the study raises important clinical and epidemiological questions.
Advertisement
"Accordingly, claims-based analyses, such as these, should be viewed as hypothesis-generating instead of categorical in nature. The electrophysiology and medical communities should look at the findings presented in this study as a motivational call to initiate prospective studies with the goal of identifying gaps in AF care, which can then be used to create effective healthcare policies, designed to reduce AF-related mortality," commented Dr. Deering and Dr. Bhimani.
Source-Eurekalert