Salivary human papillomaviruses (HR-HPV) testing will become part of routine clinical management for HPV-driven oropharyngeal cancers (OPC) patients.
‘Salivary human papillomaviruses (HR-HPV) testing will become part of routine clinical management for HPV-driven oropharyngeal cancers (OPC) patients.’





Investigators have determined that HR-HPV DNA can be detected in saliva in most patients with HPV-driven OPC at the time of diagnosis. This work highlights a potentially life-saving screening program based on salivary HR-HPV DNA testing for early cancer detection and patient monitoring. Their findings appear in The Journal of Molecular Diagnostics, published by Elsevier.
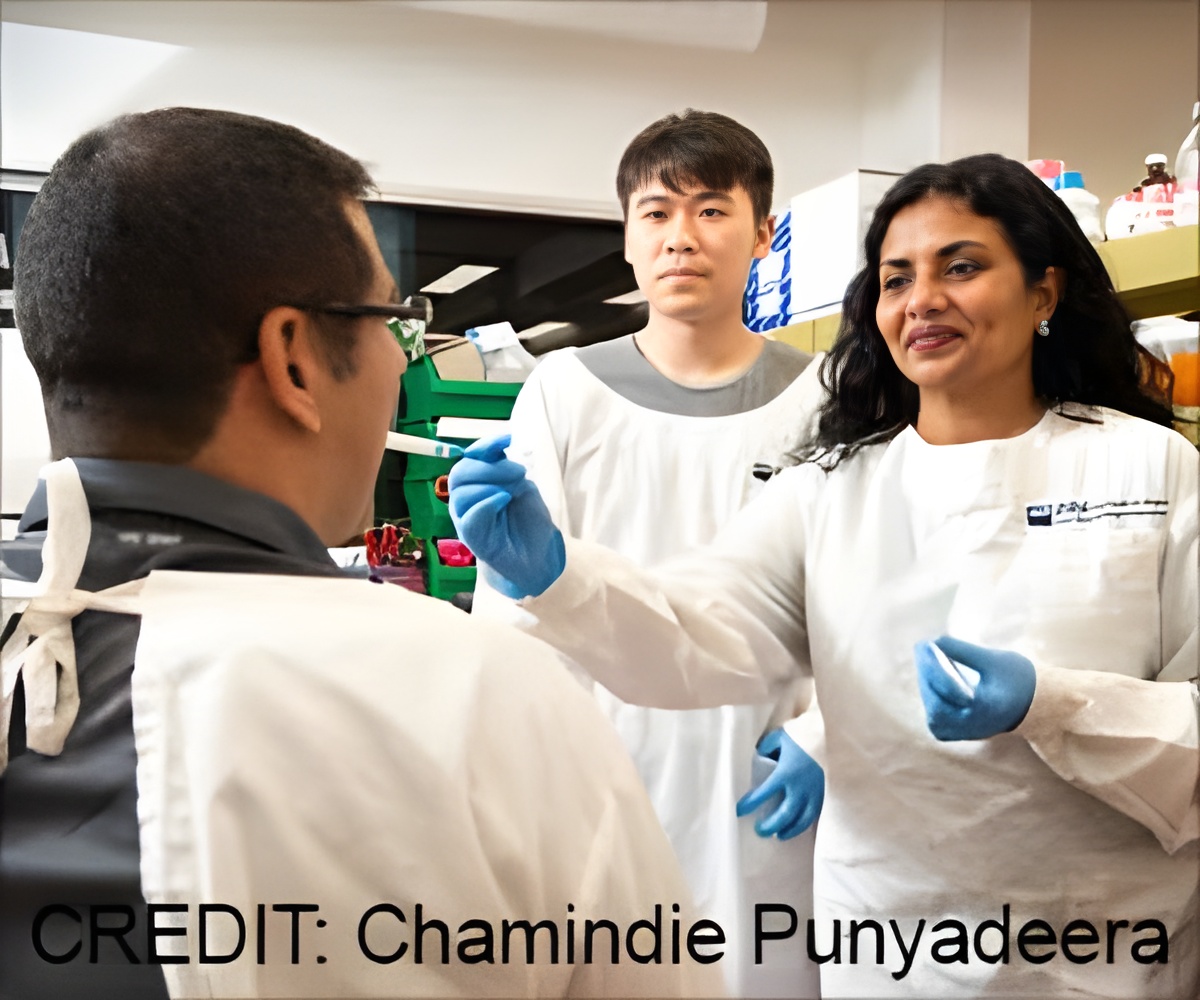
“Despite the upsurge in HPV-driven HNC, there are no early detection methods or screening strategies for this cancer type, unlike cervical cancer, which is caused by the same virus. Biomarkers enabling early detection, monitoring and disease prognostication are warranted to combat the rising incidence of HPV-driven OPC,” observed lead investigator Chamindie Punyadeera, PhD, head, Saliva & Liquid Biopsy Translational Laboratory, School of Biomedical Science, Faculty of Health, Queensland University of Technology (QUT), and Translational Research Institute, Brisbane, QLD, Australia.
Dr. Punyadeera and her colleagues investigated the efficacy of salivary HPV detection as a biomarker of HPV-HNC and survival patterns in patients with OPC to evaluate the utility of salivary HR-HPV as a prognostic biomarker for OPC.
Saliva testing was performed on 491 patients at the time of first diagnosis of HNC and 10 patients with recurring HNC. Forty-three percent were positive for salivary HR-HPV DNA. HPV16, a high-risk strain of the virus, was detected in 92% of the HPV-positive saliva samples.
Advertisement
Two hundred and fifteen patients with OPC were followed for up to five years. Salivary HR-HPV–positive patients had a clear survival advantage over their salivary HR-HPV–negative counterparts. The median event-free survivals were 205 months for HR-HPV–positive patients, compared to 82 months for HR-HPV–negative patients.
“When the noninvasive nature and convenience of the collection are considered, salivary HR-HPV testing is an ideal mode of screening asymptomatic individuals and the long-term monitoring of HPV-driven HNC patients. Our findings indicate that in the near future, salivary HR-HPV testing will become part of routine clinical management for HPV-driven OPC patients,” noted Dr. Punyadeera.
“Liquid biopsy in HNC has the potential to be truly transformative,” explained co-investigator Sarju Vasani, MD, Royal Brisbane and Women’s Hospital; and the Faculty of Medicine, The University of Queensland, Brisbane, QLD, Australia.
“It has the potential to personalize treatment selection and aid in assessing disease prognosis. It can help us select patients for adjuvant treatment and will alert us to recurrence before imaging or clinical examination has detected any specific abnormality. It is only a matter of time before these biomarkers translate from research settings to clinical practice.”
In some countries, including the United States, HNC and particularly OPC, have surpassed cervical cancers as the most common HPV-driven cancer. Patients are usually diagnosed at an advanced stage.
In the early stages, these cancers are difficult to locate with imaging studies or physical examination.
The oropharynx is difficult to access, and detection is further complicated if these smaller lesions are hidden in the crevices of the tonsils. These cancers can metastasize at an early stage, even when the primary cancer is still undetectable in size.
Source-Eurekalert