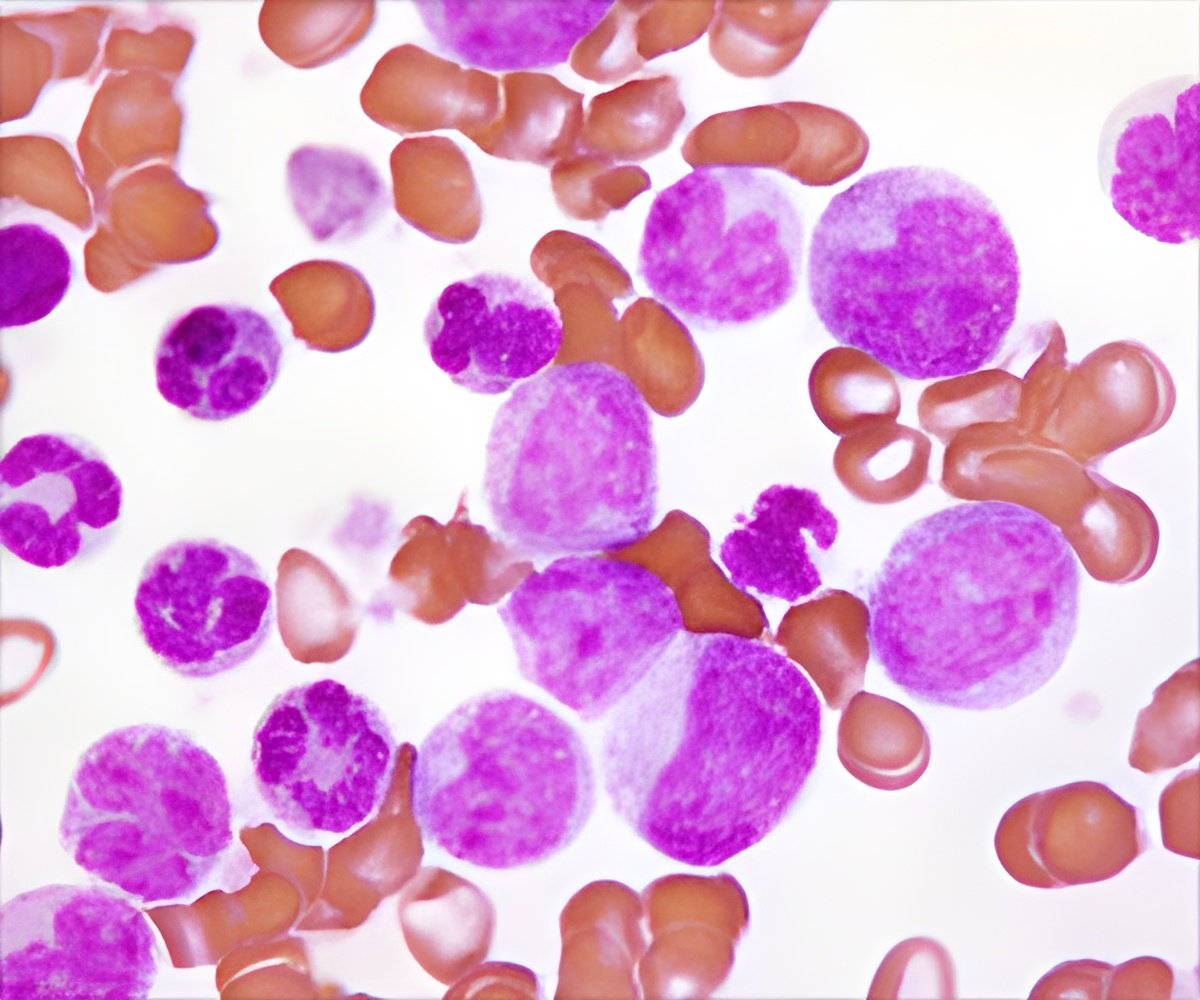
Chronic lymphocytic leukemia (CLL) is the most frequent type of cancer affecting adults in Western countries. It usually occurs in older patients.
For this purpose, the healthy B cells migrate into the B-cell zone (B-cell follicle) of the spleen and lodge there in the stromal cell niche. There they interact with follicular dendritic cells (FDC). Unlike the similarly named classical dendritic cells, the FDC are not blood cells but rather stromal cells that form a network in the center of the B cell follicle. This stromal cell network lures B cells into it and exposes them to foreign antigens, which the B cells recognize and require for their activation and maturation. Only then are they fit for their task as antibody-producing immune cells.
The B cells enter the "training center" of the lymphoid organs via the messenger molecules of the immune system, the chemokines. They guide the B lymphocytes, which have a receptor on their surface for these chemokines. Leukemia cells, as malignant immune cells, also have these homing receptors on their cell surface to which these chemokines bind, thus enabling them to establish themselves in the stromal cell niche.
In their research project, Dr. Hopken and Dr. Rehm started from the hypothesis that the processes which normally regulate the migration of B lymphocytes into the B-cell follicle are also the reason for the migration of leukemia cells into the lymphoid organs. Hence, within the B-cell follicle the survival and growth of malignant B cells may depend on the contact of the leukemia cells with the FDC.
In CLL, despite chemotherapy or radiotherapy, a relapse with renewed leukemic proliferation in lymphoid tissues can occur because the FDC usually survive chemotherapy or radiotherapy far better than the leukemia cells. If a few leukemia cells escape the therapy - physicians call this minimal residual disease - the FDC ensure that the leukemia cells within the B-cell follicles have optimal growth conditions and proliferate. Dr. Heinig, Dr. Hopken and Dr. Rehm have now elucidated this process in detail in a mouse model, which is similar to human CLL.
Intensive interaction between leukemia cells and the FDC
Advertisement
In a second step, the researchers studied the consequences of the interaction between the malignant B cells and the FDC in the B-cell follicle. The result was that the close contact between the leukemia cells and the FDC network stimulates the cancer cells to increasingly produce another signaling substance, lymphotoxin. The lymphotoxin of the leukemia cells binds to the lymphotoxin-beta receptor on the FDC, which then increasingly secrete the chemokine CXCL13. This creates a positive feedback loop because the chemokine CXCL13 plays a major role in the recruitment of leukemia cells in the B cell follicles.
Advertisement
The researchers thus identified two different targets that may complement the chemotherapy currently used to treat CLL. The first is the blockade of the chemokine/homing receptor CXCR5 on the leukemia cells, which prevents the cancer cells from lodging in the B-cell follicle. "This homing receptor," Dr. Rehm explained, "is increased on the leukemia cells of patients with CLL." Second, via the blockade of the lymphotoxin-beta receptor on the FDC, the reciprocal crosstalk between the leukemia cells and the FDC promoting tumor proliferation is interrupted and thus the tumor development is likewise significantly reduced.
From the results of their study, Dr. Rehm and Dr. Hopken infer that chemotherapies already in clinical use combined with immune therapies that interrupt the crosstalk between leukemia cells and the FDC may be beneficial. This combination could prevent the residual leukemia cells that have escaped a chemotherapy or radiation therapy from recovering in the stromal cell niche and from triggering a relapse.
Source-Eurekalert