Scientists have made an important advance in understanding the biological processes involved in cell death, which could lead to the development of new treatments for many diseases and conditions.
Scientists have made an important advance in understanding the biological processes involved in cell death, which could lead to the development of new treatments for many diseases and conditions.
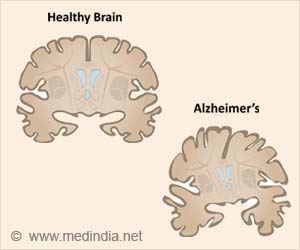
Researchers associated with the MRC Toxicology Unit at the University of Leicester point out that cells in the human body are continually dying, and most of these cells kill themselves by a form of cell death, commonly referred to as apoptosis.In a healthy body, they say, the number of cells stays constant.
Millions of new cells are produced every second, and millions of others are lost or kill themselves, the researchers state.
They even highlight the fact that failure of the normal apoptosis process plays a role in different diseases including cancer, certain neurodegenerative disorders such as Parkinson's and immune diseases, such as autoimmune lymphoproliferative syndrome (ALPS).
Dr. Marion MacFarlane of the MRC Toxicology Unit, one of the study's authors, said: "This new research takes us a step closer to understanding how the DISC triggers cells to die. The challenge now is to try and use this fundamental knowledge to help work towards finding better treatments for conditions which occur when DISC-mediated cell death goes wrong."
Studies conducted in the past have shown that a complex called the 'DISC', which is made up of different proteins and is formed following activation of molecules called 'Death Receptors', can trigger apoptosis by 'switching on' key players in the cell death process.
Advertisement
The current study has now revealed that the DISC can trigger cell death or cell survival by switching the activity of key death-promoting molecules.
Advertisement
Thus, in diseases such as ALPS, where a crucial death-promoting protein is often not active the DISC fails to function properly.
A research article describing the study has been published in the journal Molecular Cell.
Source-ANI
ARU