A therapeutic strategy targeting a specific genetic mutation that causes a common form of amyotrophic lateral sclerosis (ALS), better known as Lou Gehrig's disease has been designed.
The study, led by Professor Matthew Disney of TSRI and Professor of Neuroscience Leonard Petrucelli of the Mayo Clinic, was published online ahead of print August 14, 2014 in the journal Neuron.
"Our small molecules target a genetic defect that is by far the most major cause of familial ALS, and if you have this defect you are assured of getting ALS or FTD," Disney said. "Our findings show for the first time that targeting this mutation with a small-molecule drug candidate can inhibit toxic protein translation—and establishes that it could be possible to treat a large number of these patients, but this is just the start of these studies and additional investigations need to be done."
Currently, ALS is usually fatal two to five years after diagnosis, and there is no effective treatment for FTD, a neurodegenerative disease that destroys neurons in the frontal lobes of the brain.
Toxic Buildup
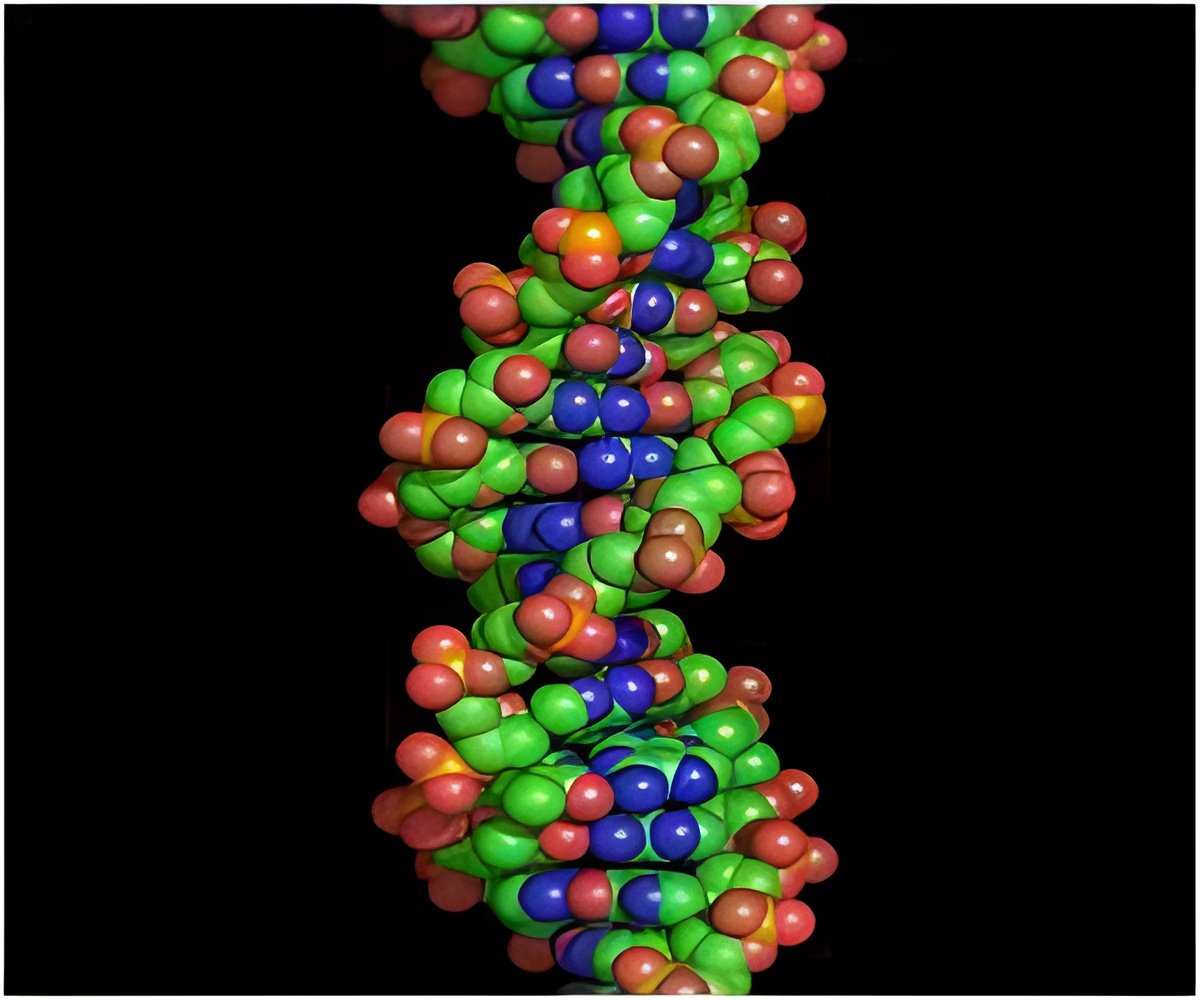
The mutation that can cause both diseases affects a gene known as C90RF72 and involves a repeat expansion, a longer than usual repetitive genetic sequence. This results in abnormal strands of RNA and the production of toxic "c9RAN proteins."
Advertisement
Two of the compounds significantly decreased levels of the toxic protein. Using a series of increasing dosages of the drug candidates, the scientists found that the highest dosage of one reduced the toxic protein by nearly 50 percent.
Advertisement
"A decrease in the levels of toxic proteins in cerebrospinal fluid in response to treatment would demonstrate the drug is working," Petrucelli said. "While additional studies must be done, this finding suggests that these proteins may provide a direct means to measure a patient's response to experimental drugs that target abnormal RNA."
Toxic proteins found in spinal fluid could also become an enrollment tool in human clinical trials, added Disney, who was enthusiastic about the collaboration with the Mayo Clinic and the larger team. "Our collective biological and chemical expertise made this research possible," he said. "This is just the beginning of what we can do together."
Source-Eurekalert











