Israeli scientists claimed to have taken skin cells from heart failure victims and turned them into heart muscle cells to repair their damaged hearts.
Even so, it marks an important advance in the quest for replacement cells to treat tissue affected by disease, said the scientists who developed the technique in Israel.
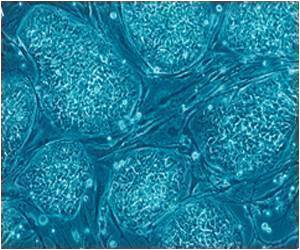
The research uses a method called human-induced pluripotent stem cells, or hiPSCs, a recently-discovered source that is viewed as an exciting and less controversial research alternative to embryonic stem cells.
It entails taking cells from a patient and introducing genes to the cell nucleus. Helped by a chemical "cocktail," these genes then act as switches which reprogramme the cells back to their versatile, youthful state.
The ultimate goal is that if a patient's own cells are used as the replenishment source, they will be recognised as friendly by the immune system and not be attacked.
Recent studies have shown it is possible to derive hiPSCs from young and healthy people and that these are capable of transforming into heart cells.
Advertisement
Nor have researchers been able to show that heart cells created from hiPSCs can integrate with existing heart tissue.
Advertisement
It is "the equivalent to the stage of his heart cells when he was just born," Gepstein said in a statement.
Gepstein's team took skin cells from two men aged 51 and 61 who had suffered heart failure and reprogrammed them by delivering three genes called Sox2, Klf4 and Oct4, followed by a molecule called valproic acid.
The method did not include a gene called c-Myc, which has roused concern because it has been found to cause tumours.
The resulting hiPSCs were cultured together with pre-existing cardiac tissue and then grafted into healthy rat hearts, where they appeared to integrate successfully.
Still unclear, though, is whether heart cells derived from the same patient will be accepted by the immune system.
"One of the obstacles in dealing with this issue is that, at this stage, we can only transplant human cells into animal models and so we have to treat the animals with immunosuppressive drugs so the cells won't be rejected," said Gepstein.
The study is published online in the European Heart Journal, published by the European Society of Cardiology.
Source-AFP