Researchers at UCLA have used an engineered common cold virus to deliver a genetic payload to prostate cancer cells in mice, which enabled them to locate the diseased cells as they spread.
Researchers at the University of California, Los Angeles (UCLA) have successfully used an engineered common cold virus to deliver a genetic payload to prostate cancer cells in mice, which enabled them to locate the diseased cells as they spread to the lymph nodes, the first place prostate cancer goes before invading other organs.
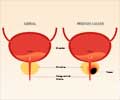
The tiny cancer metastases in the pelvic lymph nodes are very difficult to find using conventional imaging tools such as CT scanning. This discovery could aid oncologists in finding the cancer’s spread earlier, when it’s more treatable, and before it invades distant organs, said Lily Wu, a researcher at UCLA’s Jonsson Cancer Center and the senior author of the study.The next step for Wu and her colleagues is linking the non-invasive imaging advance with a treatment component, activating a toxic agent in the genetic payload to kill the spreading cancer cells. Wu hopes one day to be able to find tiny prostate cancer metastases in patients and kill them at the same time, watching it all on a PET scanner. She currently is refining this image-guided therapy in her lab in mouse models.
“I think this is very exciting for many reasons,” said Wu, who also is an associate professor of pharmacology and urology. “We now know we can reach these prostate cancer metastases at an earlier stage than before, and we know we can deliver genes to those cancer cells that produce proteins that can be imaged by PET. Now we will find out how effective this genetic toxic payload is in preventing further spread of the cancer to other vital organs.”
The study appears July 11, 2008 in the early, online edition of the peer-reviewed journal Nature Medicine.
The spread of prostate cancer to the pelvic lymph nodes is the most reliable indicator that the patient will have a poor prognosis, with disease recurrence and progression likely. Accurately assessing pelvic lymph node involvement in patients is critical in planning their treatment, Wu said.
Currently, physicians don’t know if a treatment is attacking cancer cells until, using traditional imaging, they see a decrease in tumor size, an insensitive approach that can take weeks and months. And if the treatment isn’t working, the patient is exposed to a toxic therapy that isn’t helping them. If Wu is successful, an oncologist would know within days if the cancer has spread and whether the treatment is killing the cancer.
Advertisement
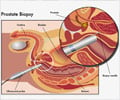
As part of this study, Wu co-developed TSTA, a two-step transcriptional amplification method, which increased the expression of the genetic payload inside the cancer cells – in effect boosting the imaging signals and potential killing activity of the engineered virus.
Advertisement
“It would represent a treatment advance in patients for whom outcome is not good,” Wu said. “This would help improve the prognosis for these patients by letting us find and treat these metastases early. If we can catch the cancer before it invades other organs, we have a better chance to change the outcomes for these patients.”
This type of approach was pioneered in the field of breast cancer with testing of the sentinel lymph node, the first place breast cancer goes when it spreads. A biopsy can determine if the cancer is in the sentinel node, therefore spreading, and oncologists base their treatment decisions on that information. In prostate cancer, the lymph nodes are much more difficult to access for biopsy, so Wu’s method provides a much needed, non-invasive alternative.
Source-Newswise
SRM







![Prostate Specific Antigen [PSA] Prostate Specific Antigen [PSA]](https://www.medindia.net/images/common/patientinfo/120_100/prostate-specific-antigen.jpg)





